Cleveland Clinic joins national trial to investigate treatment for urinary incontinence

Stress urinary incontinence (SUI), the most common type of urinary incontinence in women, carries stigma and embarrassment for many and can have a significant impact on an individual’s quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
SUI is caused by a weakening or dysfunction of the muscles and tissues that enable urethral and bladder function. Depending on the severity of the condition, there are wide-ranging interventional strategies to treat SUI — from lifestyle modifications and minimally-invasive procedures to major surgeries.
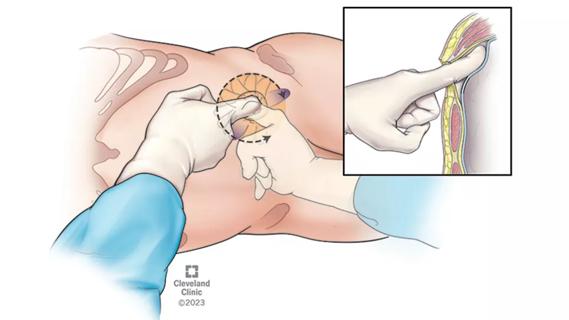
The midurethral sling (MUS) procedure is the current gold standard for the surgical treatment of SUI, wherein the surgeon makes a small incision in the vagina and inserts a synthetic strip of material under the urethra, securing it into the pelvic floor tissue.
Amid patient concerns on the use of synthetic mesh, in April 2019 the FDA asked manufacturers of transvaginal mesh intended to treat pelvic organ prolapse to halt the production and distribution of the products immediately. Medical consensus continues to favor its use in MUS to treat SUI. Still, the controversy has centered an international and national dialogue about the need for cell-based therapies to treat SUI.
A national clinical trial sponsored by Cook Myosite® is leading efforts to do just that, and Cleveland Clinic is one of the participating sites. The study is designed to evaluate the safety and efficacy of a patient’s muscle-derived stem cells in the treatment of SUI.
Howard Goldman, MD, Vice Chairman for Quality in Cleveland Clinic’s Glickman Urological & Kidney Institute and lead investigator for the Cleveland Clinic arm of the study, notes that this approach could alter the treatment paradigm for SUI.
Specifically, the double-blind randomized study will be comparing the results of a medical procedure using autologous muscle-derived cells for urinary sphincter repair (AMDC-USR) to those of placebo intervention. After an in-office muscle biopsy is taken from the participant’s thigh, the cells are processed and purified for progenitor cells, which are later injected into the patient’s urinary sphincter.
Advertisement
“The hope is that this injection will help rejuvenate, repair and restore function to the damaged cells in the sphincter,” says Dr. Goldman.
Previous research assessed the 12-month safety and efficacy of the AMDC-USR intervention and demonstrated that doses of 10, 50, 100 and 200×10(6) cells are safe in patients; however, an expanded trial size is needed to develop a more robust efficacy profile. Dr. Goldman is hopeful the data from this trial will further establish the clinical utility of this approach.
Among other criteria, eligible patients include females who are 50 to 75 years of age who have experienced moderate-to-severe symptoms of SUI for at least six months but are not interested in surgical intervention. The placebo cohort will have an opportunity to be enrolled in the AMDC-USR intervention arm of the study after one year.
“It’s a minimally invasive procedure that only requires local anesthesia and normally takes less than 15 minutes,” explains Dr. Goldman. “If the study validates its use, it could be a game-changer in the treatment of SUI, allowing a truly minimally invasive treatment utilizing no foreign material but only the patient’s own cells.”
Cleveland Clinic will begin enrolling patients later this year.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
Pioneering and refining the approach in pyeloplasty, nephrectomy and more
Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
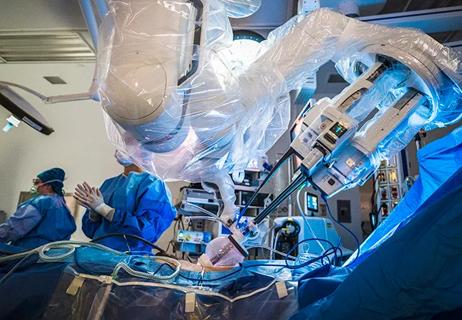
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients