Insights in the wake of a large international registry study
Infective endocarditis associated with transcatheter aortic valve replacement (TAVR) carries high rates of mortality similar to those of surgical aortic valve replacement. So finds a new international registry study of patients with post-TAVR infective endocarditis. The study has also yielded insights on the characteristics of high-risk patients, paving the way for early initiation of potentially lifesaving treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Early recognition is very important, because these patients must be treated with appropriate antibiotic therapy, says Samir Kapadia, MD, Head of Invasive and Interventional Cardiology at Cleveland Clinic and a co-author of the study, published in JAMA last month. “Even then, the mortality rate is very high.”
The study involved 20,006 patients who had undergone TAVR at 47 centers on three continents between June 2005 and October 2015. Among these patients, 250 cases of infective endocarditis were identified, representing a 1.1 incidence per person-year. The median time from TAVR to infective endocarditis was 5.3 months.
The in-hospital mortality rate among those who developed endocarditis was 36 percent. Despite treatment, 66.7 percent of patients who developed endocarditis had died at two years post-TAVR.
The following factors were found to be significantly associated with increased risk of infective endocarditis:
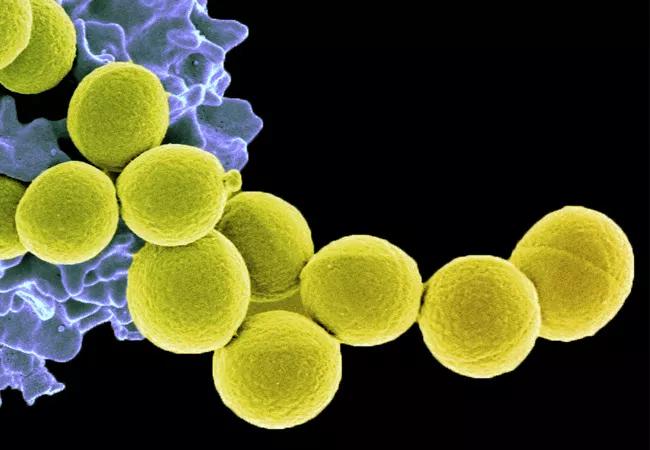
The most common pathogens identified in endocarditis cases were enterococcal species (24.6 percent of cases) and Staphylococcus aureus (23.3 percent).
The high prevalence of enterococcus surprised Cleveland Clinic infectious disease specialist Nabin Shrestha, MD, MPH. “Enterococcus is not generally the most common pathogen,” he says. “I would have expected Staphylococcus to be more common. But in TAVR, the catheter’s point of entry is the groin. Enterococcal organisms live in the gastrointestinal tract, so the most likely explanation is that the microorganisms probably entered the bloodstream during the procedure from colonization in the groin area.”
Advertisement
Staphylococcal organisms, which commonly colonize skin and mucous membranes, seed vulnerable heart valves after reaching the bloodstream through infected IV lines.
“The most important point is that many of these organisms appear to be seeded at the time of the procedure,” notes Dr. Kapadia. “This means rethinking what we do prophylactically.”
Cleveland Clinic takes multiple measures to prevent in-house acquisition of infections during TAVR, including:
While prophylactic antibiotics are considered conservative in the setting of some less-invasive procedures, Cleveland Clinic provides antibiotics to all patients undergoing cardiovascular surgery or procedures like TAVR. “The penalties of not using antibiotics are so high, and the risk of taking antibiotics is so low, that we prefer to err on the side of caution,” says Dr. Kapadia.
Patients are given IV antibiotics, including vancomycin and ciprofloxacin or similar medications, before TAVR and continued on oral antibiotics for four to five days after the procedure.
TAVR patients are closely watched, and whenever there is concern for a serious infection, Dr. Shrestha or another infectious disease specialist in the multidisciplinary Cleveland Clinic Endocarditis Center is consulted. Blood cultures are performed to detect microorganisms in the bloodstream and, when present, identify them so that an appropriate diagnosis can be made and an appropriate treatment plan formulated.
Advertisement
Whenever there is a TAVR-related infection, the team works collaboratively to ascertain how invasive it is and determine the patient’s overall condition and degree of surgical risk.
Current guidelines recommend debridement and valve replacement for patients with infected prosthetic valves and for those with highly resistant organisms or persistent bacteremia. However, surgery is not a viable alternative for many TAVR patients with infective endocarditis.
“Without valve removal, infective endocarditis can be fatal,” notes Dr. Shrestha. “Interestingly, although patients with valves placed surgically may die if an infected valve is not removed, in this study a substantial proportion of TAVR patients survived without surgery.
“When an artificial device gets infected, you cannot get rid of the infection without removing the device,” he continues. “Antibiotics can suppress the infection, but they cannot cure it. This means that in the absence of surgical removal of an infected heart valve, patients must remain on antibiotic therapy indefinitely.”
Image of Staphylococcus aureus organisms at top of post courtesy of the National Institute of Allergy and Infectious Diseases.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable