Stewardship and interpretation the difference between revolutionary and dangerous
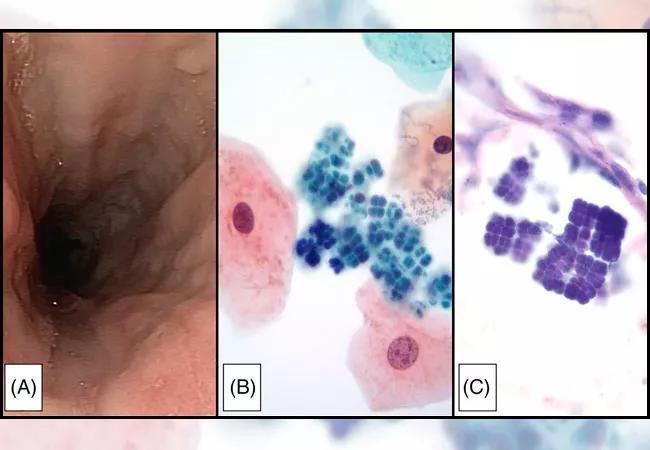
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/34690276-10ab-4968-a11b-46b06231e664/18-PTH-XXXX-sarcina-650x450_jpg)
18-PTH-XXXX-sarcina-650×450
Gary Procop, MD, MS, Director of Molecular Microbiology, Virology, Mycology and Parasitology at Cleveland Clinic, offers his take on the appropriateness of molecular sequencing and diagnostics.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
1. Recently you helped publish an article about the first documented case of Sarcina in esophageal brushing cytology. What was the importance of that discovery, and how has this impacted future molecular testing in confirming a definitive diagnosis of uncommon infections?
This is a great case to discuss, particularly in the context of advanced molecular diagnostics. It underscores when they are needed and when they are not. Sarcina (see feature image) is a bacterium that has been noted in individuals with upper gastrointestinal disorders, and a variety of associations have been proposed. In many instances, it may simply be a colonizing bacteria, as it is usually not associated with invasive characteristics or a prominent inflammatory response. This microorganism has a characteristic morphology that affords definitive identification by microscopy (i.e., metagenomic or 16S sequencing is not needed). Our prominent cytopathologist, Dr. Chuck Sturgis, who is also an excellent infectious disease pathologist, recognized this unique morphology in a cytologic preparation. The team believed it was important to bring this to the attention of other cytopathologists in the community to improve their diagnostic skills.
This specimen came from an area in the body with normal microbiota. Had polymerase chain reaction (PCR)-based 16S sequencing been performed on this specimen, then a mixed and uninterpretable sequence would likely have been obtained, because of the multiple organisms present. Had a metagenomic approach been attempted, the numerous bacterial DNA templates would have been detected, with Sarcina being only one among the many species.
Advertisement
Although we are committed to determining the optimal use of molecular diagnostics for infectious diseases, this is a great example of how traditional technology is still of great value and molecular diagnostics are not always necessary.
2. Can you discuss the validation of metagenomic next-generation sequencing tests for universal pathogen detection?
This is very exciting technology. It holds great promise as well as great danger. The danger is so significant that it could cause patient harm, which necessitates the most judicious use by providers who thoroughly understand the strengths and limitations of this technology.
The strength of this technology is reflected in an alternate name that is used, hypothesis-free testing. In short, in a metagenomic approach to diagnostics, all the nucleic acids within a specimen are sequenced, which includes human- and microbially derived nucleic acids. The human sequences are discarded, and the remaining microbial sequences present are analyzed. The identification of the microorganisms present as well as the relative quantity of each organism can be determined, if high quality databases are used. In this manner, a pathogenic organism that may not have been in the differential diagnosis may be discovered. Similarly, microorganisms that are rarely encountered, for which diagnostic tests are not available, may be detected. So, what’s the dark side of this technology?
Microorganisms are everywhere. Just because something is sterile, it is not necessarily DNA free. Buffers, specimen containers, essentially everything used to set up an assay may have contaminating microbial DNA. This, as well as background normal microbiota (i.e., normal flora) will be detected by these types of assays. Therefore, extreme care needs to be taken not to ascribe pathogenicity to bystander microorganisms. Ascribing cause to the wrong microorganism will result in diagnostic as well as treatment errors. This would lead to overuse of antimicrobial agents and promote antimicrobial resistance.
Advertisement
Finally, metagenomic assays are not as sensitive as PCR-based assays. There was recently a patient with JC virus central nervous system disease in which the JC virus was detected by a traditional PCR assay, but missed by the metagenomic assay. A metagenomic assay is broad with respect to detection, whereas PCR-based assays are deep. In summary, metagenomics using next-generation sequencing is a powerful new technology for which stewardship and results interpretation are paramount.
3. What about Cleveland Clinic’s new 16S in-house assay sequencing?
We are excited to offer sequence-based identification of bacterial pathogens direct from tissue specimens. This technology is particularly useful when cultures are negative but there is histopathologic evidence of a bacterial infection. Dr. Sandra Richter and the molecular microbiology team completed a stringent and thorough validation of this new test.
In short, the infected tissue is digested in an aseptic manner, and nucleic acids are extracted. Unlike the metagenomic assay described above, only bacterial DNA is targeted through amplification of the 16S rDNA gene. If amplification product is obtained, then DNA sequencing is performed to determine the identification of the infecting bacteria. Similar validations are underway for fungal pathogens, to be followed by validations for mycobacteria. The endocarditis team from the Department of Infectious Diseases has demonstrated the usefulness of this technology, most notably for previously treated and culture-negative endocarditis. Offering this test at our main campus has decreased the time-to-results for our patients, as well as our send-out costs.
Advertisement
Feature image: Morphology of Sarcina. A, Upper endoscopic photograph of esophagus taken at the time of brushing for Sarcina diagnosis, endoscopic impression of “esophagitis, rule out Candida,” B, Esophageal brushing with mature squamous epithelial cells and large cyanophilic cocci arranged in tetrads, S. ventriculi (ThinPrep, Papanicolaou stain, 1000×), C, Gastric mucosal biopsy taken four months prior to esophageal brushing with large, cuboidal, basophilic bacteria in tetrads, S. ventriculi (Hematoxylin & eosin stain, 1000×). Used with permission from Diagnostic Cytopathology.
Advertisement
Advertisement
The relationship between MTHFR variants and thrombosis risk is a complex issue, but current evidence points to no association between the most common variants and an elevated risk
One-time infusion of adenovirus-based therapy is designed to restore heart muscle function
Studying gender-specific health factors promises new insight into diagnosis, prognosis, treatment
Consortium is uncovering risk factors that spur disease development in an understudied group
Cleveland Clinic researchers receive $2 million grant from the National Institutes of Health
New Cleveland Clinic fellowship fosters expertise in the genetics of epilepsy
Renal genetic testing confirms diagnosis, guides management
Integrates genetic and clinical data to distinguish from GEFS+ and milder epilepsies