Skillful pre- and post-transplant care is key to success
Cardiomyopathy is an insidious disease causing vague, intermittent symptoms and a gradual decline in energy. By the time the child sees a doctor, the heart is often barely able to pump, and immediate medical attention is imperative.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Logan Martin’s story is typical. A robust, soccer-playing teenager from Dover, Ohio, Logan developed intermittent abdominal pain in 2013. When it failed to resolve after several months, his mother took him to the doctor. Abdominal tests were negative, but a chest X-ray revealed fluid in the pleural spaces and an enlarged heart. When an ECG and echocardiogram confirmed heart failure, Logan was immediately transferred to Cleveland Clinic Children’s.
“Logan didn’t realize for a long time that something was wrong, because his energy level declined very slowly,” says Robert Stewart, MD, Surgical Director of Congenital Heart Surgery at Cleveland Clinic Children’s. “Suddenly, he deteriorated very quickly.”
“When kids are transferred to our hospital, our first job is to stabilize them,” says Gerard Boyle, MD, Medical Director of Pediatric Heart Failure and Transplant Services.
If they have difficulty breathing on their own, a cardiac anesthesiologist is called to insert a breathing tube. CPR is performed if the heart stops or slows dramatically. As a safety precaution, Dr. Stewart and his team stand by to support the patient with extracorporeal membrane oxygenation (ECMO) if it is necessary.
After intubation, patients generally require a couple of days to stabilize. When all goes well, a gradual transition to oral medication is accomplished. “This is often not the case, and we have to list the patient for transplant right away,” says Dr. Boyle.
Logan was diagnosed as having dilated cardiomyopathy with left ventricular noncompaction. He was treated with oxygen, a diuretic and IV milrinone.
Advertisement
When patients are referred early, medical therapy may prevent deterioration and transplantation. “Heart transplantation is not a cure,” says Dr. Boyle. “It carries risks of its own. We help patients keep their own hearts as long as possible before subjecting them to the potential complications of the transplant procedure and the antirejection medications.”
For patients like Logan, meticulous medical management helps promote survival until a donor heart can be found.
Logan was hospitalized for about 36 hours when he exhibited signs of stroke. The stroke team took immediate action. A CT revealed a clot in Logan’s left middle cerebral artery. He was taken to the neuro-interventional suite, where the clot was extracted with a specialized catheter equipped with pincers.
“Thanks to these resources,” says Dr. Boyle, “we were able to identify and extract the clot within an hour of Logan’s first symptoms. Within three hours, he was back in his room and fully functional.”
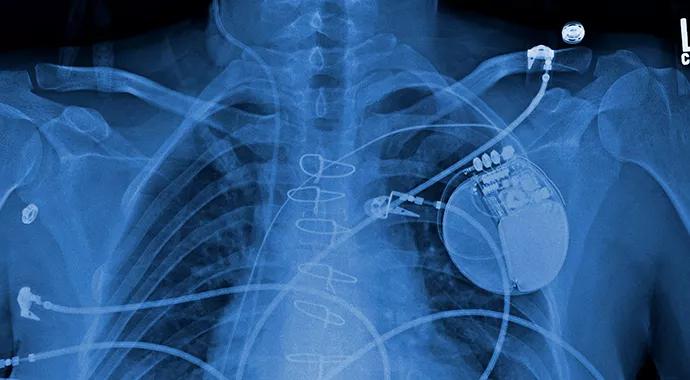
Despite maximum medical therapy, Logan’s heart failure worsened. At this point, his cardiologists believed he might benefit from a left ventricular assist device (LVAD).
Three LVADs are available for pediatric patients. All require careful management of anticoagulation.
Logan was given a third-generation HeartWare® VAD. He began to gain lean body mass almost immediately and was able to begin physical therapy. As a result, he was in good condition to tolerate the transplant when a donor heart arrived six weeks later.
Logan was transplanted in April 2014 and has fared well since, recovering quickly and graduating from high school on time despite having missed seven months of classes.
Advertisement
His was one of five pediatric heart transplants performed at Cleveland Clinic Children’s in the first seven months of 2014, bringing the total to 145 since Cleveland Clinic’s pediatric heart transplant program began in 1985.
But the true measure of a heart transplant program is not how many patients are transplanted but how well they do before and after surgery. In this arena, Cleveland Clinic Children’s patient survival and graft survival rates are routinely at or above national averages and severity- adjusted expected levels. Moreover, its pediatric cardiologists have successfully bridged four young children to transplant using the Berlin Heart Excor® LVAD without a single pump-related major complication.
Dr. Boyle will continue to monitor Logan’s progress for life, as he does for most of his patients. Nearly 75 pediatric heart transplant recipients are still being followed by Cleveland Clinic Children’s cardiologists.
Exceptions are patients who develop conditions that require the expertise of adult-care cardiologists, such as becoming pregnant while taking antirejection medications. Because patients have typically developed a tight bond with their pediatric cardiologist, a transition specialist helps them develop confidence in their new care team.
Meanwhile, Drs. Boyle and Stewart meet regularly with colleagues from Ohio’s other two pediatric heart transplant programs and discuss every patient they wait-list or transplant. “The more we share, the more we learn from our collective experience,” says Dr. Stewart.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable