Study shows benefit for stage 3, not stage 4, CKD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic kidney disease (CKD) is a worldwide public health problem that affects millions of Americans. Patients with CKD have an increased risk of mortality in general and cardiovascular mortality in particular. Specifically, as the stage of CKD progresses, patients are more prone to developing sudden cardiac death (SCD).

Recent advances in medicine and technology have led to the development of implantable cardioverter-defibrillators (ICDs), which are devices capable of detecting arrhythmias and delivering corrective electric shocks.
In the general population, the benefits of ICDs in preventing sudden cardiac death are now well-proven. Since patients with CKD appear to die more frequently from SCD, the intuitive assumption is that this population would gain significantly from ICDs. Unfortunately, the major studies that established the indications for ICD placement excluded patients with chronic kidney disease, so the benefits in this population remain uncertain.
In the last few years, Cleveland Clinic has developed a large CKD registry comprising more than 50,000 patients. The registry is serving as a key research tool, shedding light on numerous matters related to CKD care.
We used our CKD registry to identify patients who had an ICD placed for primary prevention between Jan. 1, 2001, and Oct. 31, 2011.
Demographic details were extracted from the electronic health record (EHR). The primary outcome of interest (all-cause mortality) was ascertained from our EHRs and linkage of our CKD registry with the Social Security Death Index. Patients were followed from their date of study entry (date of second qualifying estimated glomerular filtration rate (eGFR) or first ICD) until Oct. 31, 2011.
Advertisement
We then developed a propensity score of the likelihood of receiving an ICD, utilizing the following variables: age, sex, race, diabetes, hypertension, malignancy, body mass index, coronary artery disease, coronary revascularization, congestive heart failure, ventricular arrhythmia, cerebrovascular disease, eGFR, left ventricular ejection fraction, and use of renin-angiotensin system blockers, statins and beta blockers. We used one-to-one greedy matching with 0.1 caliper width to match patients with an ICD to those without.
We included 1,053 patients who had an ICD placed for primary prevention. We identified 9,435 potential controls for those with an ICD. Patients with an ICD were more likely to be younger, to be men, and to have lower ejection fraction, diabetes, congestive heart failure and coronary artery disease than were those with no ICD. As expected, there was a higher incidence of arrhythmia in the ICD group. We were able to match 631 of 1,053 patients (60 percent) with an ICD with 0.1 calipers.
Among the 1,262 matched cases and controls, there were 578 deaths during a median follow-up of 2.9 years. Figure 1 shows a Kaplan-Meier plot of survival by ICD among matched patients with different eGFR categories. After propensity score matching, ICD was associated with significantly lower mortality among those with an eGFR < 60 mL/min/1.73 m2 in both the unadjusted and adjusted models.
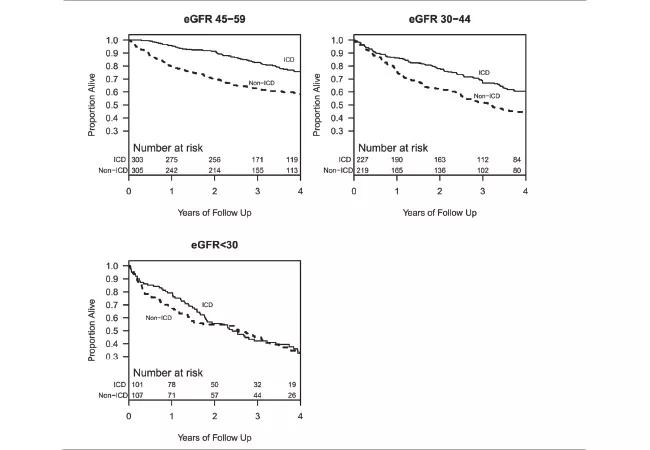
Figure 1. Kaplan-Meier curves showing survival of those with and without an implantable cardioverter-defibrillator (ICD) for various estimated glomerular filtration rate (eGFR) categories. Republished with permission of the Clinical Journal of the American Society of Nephrology, from: Implantable cardioverter-defibrillators in patients with CKD: a propensity-matched mortality analysis. Nakhoul GN, Schold JD, Arrigain S, et al. 2015 Jul 7;10(7):1119-1127. Permission conveyed through Copyright Clearance Center, Inc.
Advertisement
We found a significant interaction (p = 0.04) between ICD and an eGFR of 45-59 mL/min/1.73 m2 and an eGFR of 30-44 mL/min/1.73 m2, in which patients with an ICD and an eGFR within these two intervals had a significantly lower hazard of mortality, with hazard ratios of 0.58 (95 percent confidence interval [CI], 0.44-0.77) and 0.65 (95 percent CI, 0.50-0.85), respectively. No such association was noted among those with an eGFR < 30 mL/min/1.73 m2.
The major finding from our study is that the presence of an ICD was associated with lower mortality in patients with stage 3 CKD, but not among patients with stage 4 CKD.
Our study is one of the few to examine the benefits of ICD per CKD stage and offers the advantage of a large number (the largest to our knowledge) of patients with eGFR < 30 mL/min/1.73m2. More importantly, it is so far the only study that includes a control group.
Confirming the survival benefits of ICD placement in stage 3 CKD patients is crucial because this category constitutes the vast majority of non-dialysis-dependent CKD. We believe that the lack of protective effects of ICDs among stage 4 CKD patients could be due to the higher presence of comorbidities in this cohort.
While preliminary evidence appears to support this hypothesis, it is too early to draw definitive conclusions. However, our results suggest that ICD implantation should be considered carefully in patients with advanced CKD. Additional clinical trials examining the benefits and other complications of ICDs are warranted to support ICD placement in stage 4 CKD populations.
Advertisement
In summary, in a large cohort matched for demographics, comorbidities, and cardiac and kidney function, the presence of an ICD was associated with lower mortality in those with stage 3 CKD, but not in those with stage 4 CKD.
Dr. Nakhoul is an associate staff member of the Department of Nephrology and Hypertension in Cleveland Clinic’s Glickman Urological & Kidney Institute.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable