Tissue destruction differs dramatically by organism

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
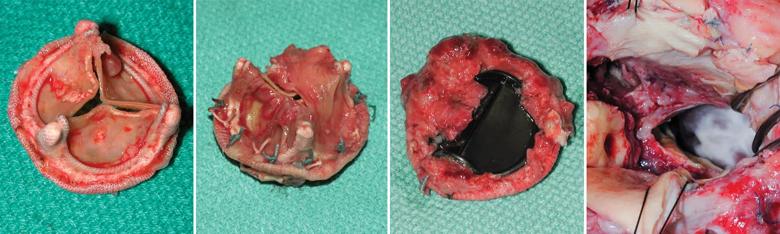
The organisms causing infective endocarditis are not equally destructive or invasive, as made clear by the four images above.
The explanted tissue valve in Panel 1 was infected with a less-aggressive organism such as an Enterococcus species. Such organisms are generally minimally invasive, causing formation of small vegetations, with recurrent episodes of sepsis.
In contrast, aggressive organisms, such as Staphylococcus aureus, can cause rapid, extensive tissue destruction, usually within a few weeks, with formation of large vegetations. Panels 2 to 4 show a tissue valve (2) and a mechanical valve (3) infected by S. aureus and extensive tissue destruction with aortic root abscess (4) caused by S. aureus prosthetic valve endocarditis.
Additional revealing image series are available in the atlas of infective endocarditis published in the April 2014 Journal of Thoracic and Cardiovascular Surgery by Cleveland Clinic cardiothoracic surgeons Gösta Pettersson, MD, PhD, and Syed Hussain, MD, and detailed here on Consult QD.
“The atlas presents major concepts that collectively describe the main features and basic facts about endocarditis every surgeon needs to know,” Dr. Pettersson says.
The concepts are:
Advertisement
Contact Dr. Pettersson at petterg@ccf.org and Dr. Hussain at hussais2@ccf.org.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable