Novel bioprosthesis offers leaflet exchangeability for multiple benefits
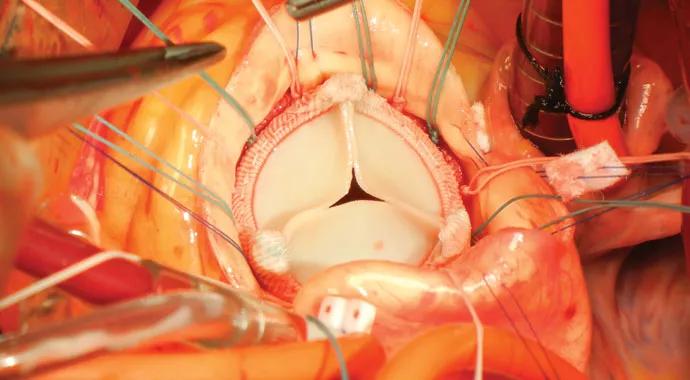
The following intraoperative images show essential steps in the implantation of a promising advance in aortic valve replacement: the advent of a two-part aortic bioprosthetic valve — namely, the ValveXchange Vitality™ aortic bioprosthesis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This novel approach involves surgical placement of the valve’s base in the aortic root (first image above) followed by installation of a tri-leaflet set (three bovine pericardium tissue leaflets mounted on a circular frame) on top of the base (second image above). The two component parts of the bioprosthesis are depicted below.
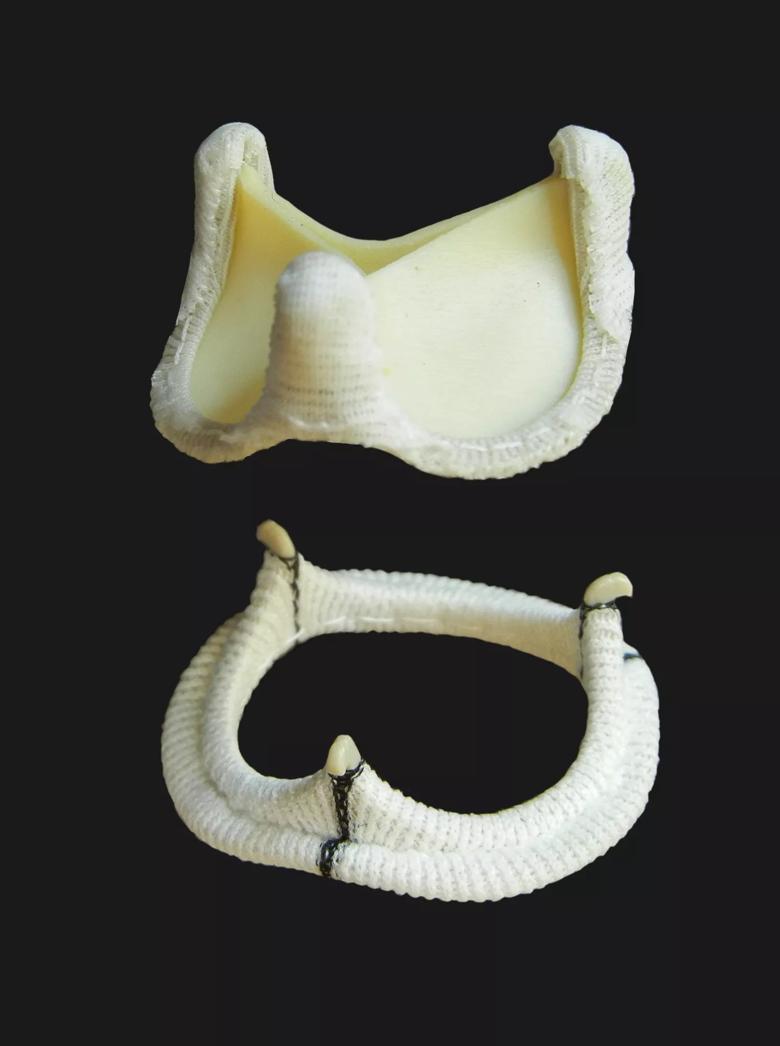
Several objectives drove this two-part valve design, including:
The latter objective of leaflet exchangeability becomes increasingly desirable as patients receive tissue valves at ever-younger ages and live increasingly long and active lives (see related post). In these cases, if a reoperation is eventually needed to replace a worn-out tissue valve, only the leaflet (not the base) needs to be replaced, which can be done less invasively and more quickly than full bioprosthetic replacement.
Cleveland Clinic surgeon and Heart & Vascular Institute Chair Lars G. Svensson, MD, PhD, implanted the first Vitality aortic bioprosthesis in a human in September 2011, and Cleveland Clinic continues to play a lead role in studying the device, which is approved for use in Europe but still investigational in the United States.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable