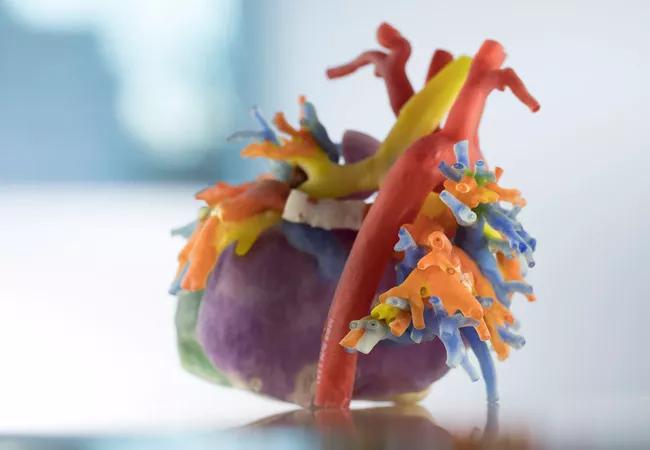
3-D replica informs an innovative operation in a deeply cyanosed child
By Patcharapong Suntharos, MD, and Hani Najm, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ethan is a 9-year-old boy with heterotaxy syndrome that was characterized by complex congenital heart disease involving the following:
As an infant, he underwent TAPVR repair with anastomosis of the pulmonary venous confluence to the right side of the common atrium followed by unifocalization of his MAPCAs to a 12-mm aortic homograft-valved conduit connected to the right ventricle. He later underwent nine cardiac catheterizations, mainly to alleviate significant pulmonary artery branch stenoses and augment pulmonary artery blood flow. Nevertheless, he still had profound cyanosis.
In July 2016, we needed to innovate a procedure to improve oxygen saturation values in this deeply cyanosed child, but standard imaging modalities were inadequate for surgical planning. Building on Cleveland Clinic’s experience developing 3-D-printed heart replicas to plan transcatheter pulmonary valve implantations in patients with congenital defects, we decided to generate a 3-D-printed model of Ethan’s heart to assist our planning.
Using contrast-enhanced MRIs and CTs of his heart, we developed the 3-D-printed model shown above, which allowed us to examine the probability of whether a procedure could improve his oxygen saturations. When the surgeon (co-author Hani Najm, MD) was able to hold the exquisitely detailed heart replica in hand and make an incision in it, the feasibility of our proposed novel procedure was demonstrated.
Advertisement
That procedure was executed in real life exactly as planned on the 3-D replica, and the outcome was excellent. Ethan is now doing very well, with saturation percentages in the low 90s — a level he had never achieved before.
3-D-printed heart replicas are exceptional tools for planning percutaneous and surgical interventions for complex congenital heart defects. Our team looks forward to more opportunities to apply this technology in previously untreatable cases.
Dr. Suntharos is a pediatric and congenital interventional cardiologist, and Dr. Najm is Chair of Pediatric and Congenital Heart Surgery, both at Cleveland Clinic.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable