Its vascular consequences
By Georges N. Nakhoul, MD, Stacey Jolly, MD, MAS, FACP, and Hernan Rincon-Choles, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The balance between dietary intake and excretion of phosphorus can be impaired in patients with decreased renal function, leading to hyperphosphatemia. Many patients with end-stage renal disease on dialysis require phosphorus-binding drugs to control their serum phosphorus levels.
In a previous post, we discussed the pathophysiology of hyperphosphatemia in kidney disease. Here we discuss its consequences.
Elevated serum phosphorus levels (normal range 2.48–4.65 mg/dL in adults) are associated with cardiovascular calcification and subsequent increases in mortality and morbidity rates. Elevations in serum phosphorus and calcium levels are associated with progression in vascular calcification and likely account for the accelerated vascular calcification that is seen in kidney disease.
Hyperphosphatemia has been identified as an independent risk factor for death in patients with end-stage renal disease, but that relationship is less clear in patients with chronic kidney disease. A study in patients with chronic kidney disease and not on dialysis found a lower mortality rate in those who were prescribed phosphorus binders, but the study was criticized for limitations in its design.
Hyperphosphatemia can also lead to adverse effects on bone health due to complications such as renal osteodystrophy.
However, in its 2017 update, the Kidney Disease: Improving Global Outcomes (KDIGO) program only “suggests” lowering elevated phosphorus levels “toward” the normal range in patients with chronic kidney disease stages G3a through G5D, i.e., those with glomerular filtration rates less than 60 mL/min/1.73 m2, including those on dialysis. The recommendation is graded 2C, i.e., weak, based on low-quality evidence (https://kdigo.org/guidelines/ckd-mbd).
Advertisement
Diet is the major source of phosphorus intake. The average daily phosphorus consumption is 20 mg/kg, or 1,400 mg, and protein is the major source of dietary phosphorus.
In patients with stage 4 or 5 chronic kidney disease, the Kidney Disease Outcomes Quality Initiative recommends limiting protein intake to 0.6 mg/kg/day. However, in patients on hemodialysis, they recommend increasing protein intake to 1.1 mg/kg/day while limiting phosphorus intake to about 800 to 1,000 mg/day. This poses a challenge, as limiting phosphorus intake can reduce protein intake.
The phosphorus-to-protein ratio reflects the phosphorus content of protein-rich foods. A phosphorus-to-protein ratio of less than 10 mg/g helps to balance adequate protein intake while preventing hyperphosphatemia. Egg whites, for example, have a phosphorus-to-protein ratio of 2 mg/g.
Sources of protein can be broadly classified as plant-based or animal-based. Animal protein contains organic phosphorus, which is easily absorbed. Plant protein may not be absorbed as easily.
Moe et al studied the importance of the protein source of phosphorus after seven days of controlled diets. Despite equivalent protein and phosphorus concentrations in the vegetarian and meat-based diets, participants on the vegetarian diet had lower serum phosphorus levels, a trend toward lower 24-hour urinary phosphorus excretion, and significantly lower FGF23 levels than those on the meat-based diet. This suggests that a vegetarian diet may have advantages in terms of preventing hyperphosphatemia.
Advertisement
Another measure to reduce phosphorus absorption from meat is to boil it, which reduces the phosphorus content by 50 percent.
Processed foods containing additives and preservatives are very high in phosphorus and should be avoided, particularly as there is no mandate to label phosphorus content in food.
Although hemodialysis removes phosphorus, it does not remove enough to keep levels within normal limits. Indeed, even when patients adhere to a daily phosphorus limit of 1,000 mg, phosphorus accumulates. If 70 percent of the phosphorus in the diet is absorbed, this is 4,500 to 5,000 mg in a week. A four-hour hemodialysis session will remove only 1,000 mg of phosphorus, which equals about 3,000 mg for patients undergoing dialysis three times a week, far less than phosphorus absorption.
In patients on continuous ambulatory peritoneal dialysis, a daily regimen of four exchanges of 2 L per exchange removes about 200 mg of phosphorus per day. In a 2012 study, patients on nocturnal dialysis or home dialysis involving longer session length had greater lowering of phosphorus levels than patients undergoing routine hemodialysis.
Hence, phosphorus binders are often necessary in patients on routine hemodialysis or peritoneal dialysis.
In caring for patients with chronic kidney disease, it is important to prevent and treat hyperphosphatemia with a combination of dietary restrictions and phosphorus binders. In a previous post, we discussed the pathophysiology of hyperphosphatemia in kidney disease. Here we discuss its consequences. A future post will discuss its control and the different classes of phosphorus binders with respect to their availability, cost, side effects and scenarios in which one class of binder may be more beneficial than another.
Advertisement
This abridged article was originally published in Cleveland Clinic Journal of Medicine.
Dr. Rincon-Choles is staff in the Department of Nephrology and Hypertension. Dr. Jolly is staff in the Department of Internal Medicine. Dr. Nakhoul is Director of the Center for Chronic Kidney Disease in the Department of Nephrology and Hypertension.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
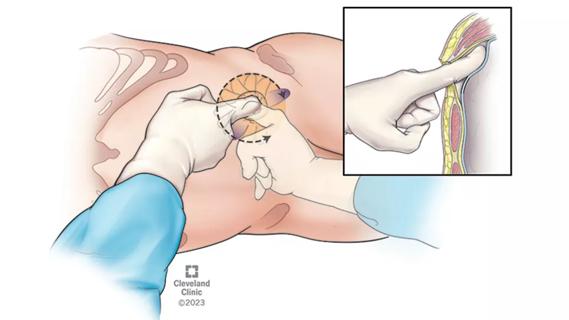
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
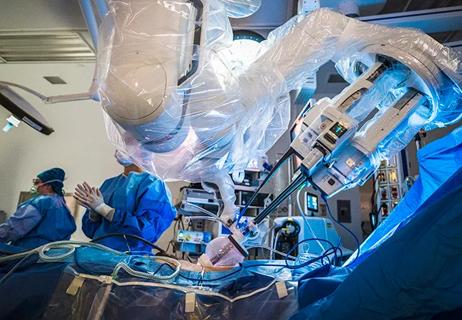
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients