New study evaluates the most popular products

Male factor infertility can be due to hormonal, genetic or anatomic causes or oxidative stress. But in up to 25% of patients, the condition is idiopathic. That’s one reason why so many men turn to over-the-counter pills and capsules with ambiguous claims of improving sperm health.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Male fertility supplements are readily available online, in drug stores and health food stores, without prescriptions,” says Neel Parekh, MD, a Cleveland Clinic urologist and male fertility specialist. “The problem is because they’re supplements, they don’t undergo the same scrutiny by the FDA as medications.”
While many of these supplements claim to be ‘clinically proven,’ are they really? And how effective are they at improving male fertility? Dr. Parekh recently co-authored an article that analyzed the scientific evidence.
It’s the first study to evaluate male fertility supplements in a comprehensive way, he says.
In the study, recently published in Urology, Dr. Parekh and colleagues looked at 17 of the most commonly used male fertility supplements from popular online retailers. These supplements contained 90 unique ingredients, which researchers graded by level of published evidence:
Of the 90 ingredients, only 20 (22%) had any published evidence regarding sperm parameters and live birth rates. And only 15 (17%) actually showed a positive effect, receiving either an A or B letter grade.
Ingredients with the best-proven effectiveness were:
Advertisement
Researchers then assigned a numerical score to each letter grade (A=5, B=3, C=0, D=-1) and calculated a composite score for each male fertility product, which contained between 1 and 46 ingredients. With the highest possible score of 5.0, the average score of all 17 products analyzed was 1.66.
“We were surprised at the lack of evidence behind the vast majority of ingredients in male fertility supplements,” says Dr. Parekh. “Most supplements are unproven and should be taken with caution.”
Taking supplements unnecessarily, especially taking more than the Recommended Dietary Allowance, can cause a host of health problems.
“We see it all the time,” says Dr. Parekh, noting that excessive levels of iron, zinc, calcium and vitamin C may lead to gastrointestinal problems. Similarly, high levels of vitamin D and vitamin C may increase the likelihood of kidney stones, and excessive vitamin B6 can lead to neuropathy.
Ironically, high levels of some ingredients — namely antioxidants — commonly found in male fertility supplements can cause infertility in some men. Reductive stress, a condition detrimental to sperm health and embryogenesis, occurs when antioxidants in the body outnumber reactive oxygen species, unbalancing the body’s natural homeostasis.
“Male oxidative stress infertility (MOSI) [when reactive oxygen species outnumber antioxidants] is really the only condition that can be treated effectively with male fertility supplements,” says Dr. Parekh. “Men with MOSI have no underlying cause of infertility other than markers of oxidative stress in their semen analysis. For them, taking supplemental antioxidants for three months or longer can improve sperm parameters. If a patient doesn’t have MOSI, however, taking antioxidants may do more harm than good.”
Advertisement
Male fertility supplements aren’t for every man wrestling with infertility. They aren’t for most, stresses Dr. Parekh.
“It’s important for patients to see a male fertility specialist who can conduct a comprehensive exam and accurately diagnose the causes of infertility so they can be treated appropriately,” he says. “That’s the best place to start, instead of falling for false advertising online and potentially causing more harm.”
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
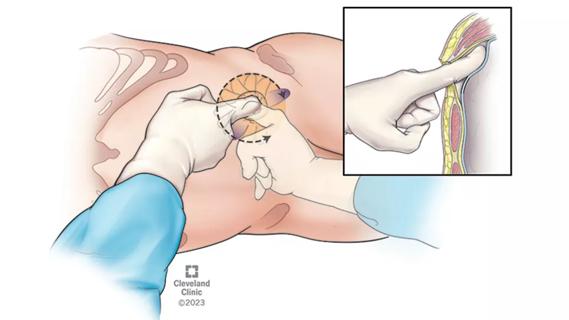
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
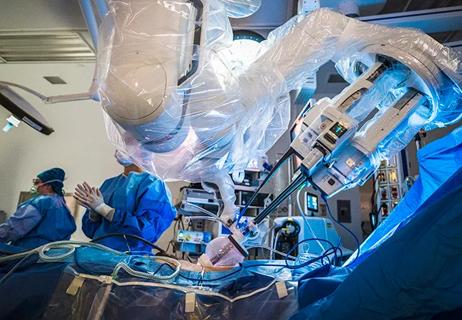
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients