Review says there’s too much data variance to know
Useful comparative evidence for the durability of bioprosthetic aortic valves is lacking because of the wide variability of data collected between various studies and reports. That’s the conclusion of the most comprehensive literature review to date focused on structural valve deterioration (SVD) of surgical bioprosthetic aortic valves. The analysis was published online in JAMA Cardiology December 5 by a team of Cleveland Clinic researchers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our review found vastly different follow-up periods and end points, as well as the use of no fewer than 11 different definitions of structural valve deterioration,” says the study’s corresponding author, Samir Kapadia, MD, Section Head of Invasive and Interventional Cardiology at Cleveland Clinic. “The lack of standard data collection precludes comparisons and meta-analyses.”
Although bioprosthetic aortic valves are less durable than their mechanical counterparts, they are increasingly used because of mechanical valves’ requirement for lifelong anticoagulation with its accompanying risk of bleeding complications. Nevertheless, the durability of the various bioprosthetic valves used clinically is unknown. Although many studies have reported on SVD, comparisons between available devices are difficult to make because of inconsistent data collection among studies.
To better understand the limitations of current evidence, the Cleveland Clinic investigators performed a systematic review of published literature through November 2016 with the goal of capturing all available studies on the durability of surgical bioprosthetic aortic valves. They found and analyzed 167 studies and 12 FDA reports, which collectively included 101,650 patients and 17 different valve types.
Wide variability was found among the studies in multiple parameters:
Advertisement
Moreover, SVD definitions were inconsistent between studies, with some based on clinical factors (e.g., symptoms of heart failure, echocardiographic parameters or reoperation) and others on morphological deterioration of the valve (e.g., wear, calcification, leaflet tear, stress fracture or stent creep), in varying combinations.
Another surprising finding, according to the authors, was that only 11 studies (6 percent) reported core laboratory data, with the longest core laboratory follow-up being just five years.
“The result of poor data is that it leaves us with no reliable benchmark for valve deterioration,” says cardiothoracic surgeon Lars Svensson, MD, PhD, Chair of Cleveland Clinic’s Miller Family Heart & Vascular Institute and a co-author of the study. “Having a standard is critically important, not only for comparing existing valves but also as a benchmark against which to measure new valves and transcatheter devices as they are developed.”
The authors point out the particular importance of collecting long-term follow-up data for evaluating SVD in aortic valves. Multiple studies show that SVD risk decreases with increasing patient age at implantation. As increasing numbers of younger patients opt for a bioprosthetic valve to avoid lifelong anticoagulation therapy, a firm understanding of age-related risk is critical.
Standardizing definitions of SVD for bioprosthetic aortic valves should be another important priority, the authors note, and they identify two recent reports that include proposals for doing so:
Advertisement
Finally, the authors of the literature review recommend that long-term core laboratory analysis be standard practice for studies.
“With so many valves in use and more options becoming available all the time, we must have a way to compare them,” concludes Dr. Kapadia. “For physicians to make evidence-based decisions, studies need to adopt an approach with long-term and complete data collection, standardized methodologies and uniform definitions.”
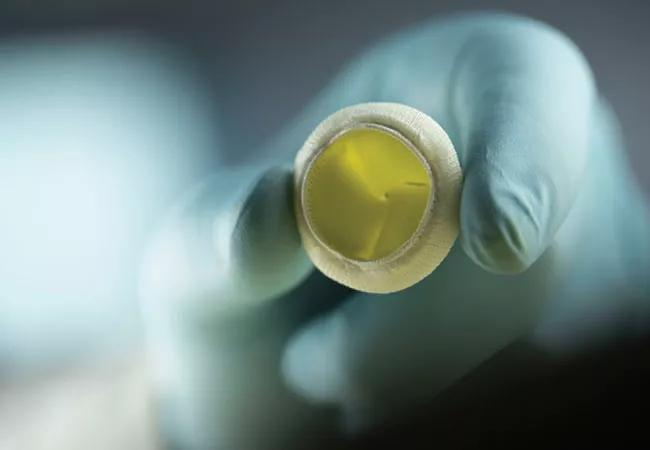
Photo credit: © Russell Lee
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable