Latest systems combine continuous glucose monitoring with automatic basal insulin delivery

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/911e0692-4a99-4942-b709-c56c0f3ce5d9/20-HVI-1961367-CQD-interventions-cardiometabolic-disorders-Hero_jpg)
20-HVI-1961367-CQD-interventions-cardiometabolic-disorders-Hero
Current FDA-approved closed-loop digital systems with the capability to automatically deliver basal insulin based on glucose levels are putting diabetes management increasingly in the hands of patients — and improving outcomes in the process. So reports preventive cardiologist Dennis Bruemmer, MD, PhD, in a recent Cleveland Clinic Tall Rounds online CME activity on digital health in cardiovascular medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Digital technology has been embraced in diabetes care for decades,” says Dr. Bruemmer, Director of Cleveland Clinic’s Center for CardioMetabolic Health. “Sophisticated devices have recently become available that are extending the time of euglycemia while reducing risk of hypoglycemia.”
Dr. Bruemmer reminds his colleagues that the majority of patients presenting to cardiologists have diabetes and that the condition is poorly controlled in most cases. He urges cardiologists to become well versed in comprehensive diabetes management, including managing medications with proven cardiovascular benefit, continuous glucose sensing, insulin pump therapy, and closed-loop sensing and insulin delivery systems.
Among patients presenting with acute coronary syndrome, he notes, about one-quarter have a hemoglobin A1C level above 9%. This group is more likely to suffer worse outcomes, including death. Hence, patients with a diagnostic hemoglobin A1C of above 9% should be treated with insulin.
“Cardiologists are actually involved in the care of patients with diabetes more often than doctors in other specialties, including endocrinologists,” he says. “More than one-third of patients presenting to cardiologists are treated with insulin, so it is critical that we be aware of the newest technologies and be actively involved in insulin management.”
In his Tall Rounds talk, Dr. Bruemmer briefly outlines the history of glucose monitoring and insulin therapy since its beginnings in the 1920s. The technology has advanced dramatically over the years, with a particular uptick in the past five years that has revolutionized care and improved patient outcomes.
Advertisement
In the 1940s, glucose was tested with glucose oxidase technology, requiring multiple complex steps. The first glucometer was introduced in the 1970s. Now fingerstick glucose monitoring linked to an iPhone is available, as are continuous glucose-sensing devices.
Likewise, insulin delivery technology has undergone dramatic recent changes. The first insulin pump — a large backpack-like device — was developed in the 1960s. It was actually a very sophisticated system, Dr. Bruemmer notes, using infusions of both insulin and glucagon, which remain contemporary care today. In the late 1970s, the first small insulin pump was introduced, which delivered small amounts of fast-acting insulin continuously throughout the day. We now have an insulin pump system that uses iPhone-like technology that links with all our daily devices and automates insulin delivery.
The idea to link continuous glucose monitoring data to continuous subcutaneous insulin infusion therapy was introduced in the early 2000s and notably expanded since then, with the first “artificial pancreas” developed in 2009.
Such combined glucose-sensing and insulin delivery devices are now FDA-approved and available, using closed-loop systems consisting of a continuous under-the-skin glucose sensor connecting to an insulin delivery system to automatically supply the correct dose of insulin based on computer algorithms. The system essentially takes over glucose measurements and adjusts basal insulin delivery. Recent evidence shows that patients with type 1 diabetes using such systems are achieving more time in euglycemia and a reduced risk of hypoglycemia (N Engl J Med. 2019;381:1707-1717).
Advertisement
Not surprisingly, Dr. Bruemmer adds, a technologically adept segment of the diabetes patient community is sidestepping FDA approval of new devices and is well organized to guide one another online in what’s known as “DIY looping.” These patients use available auto-looping algorithms that can essentially connect any diabetes device with glucose sensing and insulin delivery.
With the help of Leslie Cho, MD, Co-Section Head of Preventive Cardiology and Rehabilitation, Dr. Bruemmer has cleared the way for data from the FDA-cleared and HIPAA-compliant Glooko mobile app to soon be integrated into Cleveland Clinic’s electronic health record to inform patient management. Patients use the app to sync data from compatible blood glucose monitors, insulin pumps and continuous glucose monitors to their smartphone. From there, data can be transferred via a cloud-based platform to the patient’s care provider.
The app generates data reports (Figure) that are critical for patients to learn about and manage their diabetes, covering both glucose-sensing activity and nutritional data. For example, a patient may be able to quickly glean from her data that she may need to bolus earlier before her next meal and do so with more than her usual insulin dose.
“It’s not just important for the physician to manage and see patient data,” says Dr. Bruemmer. “Enabling patients to see their trends in user-friendly formats can be very empowering and lead to better self-management.”
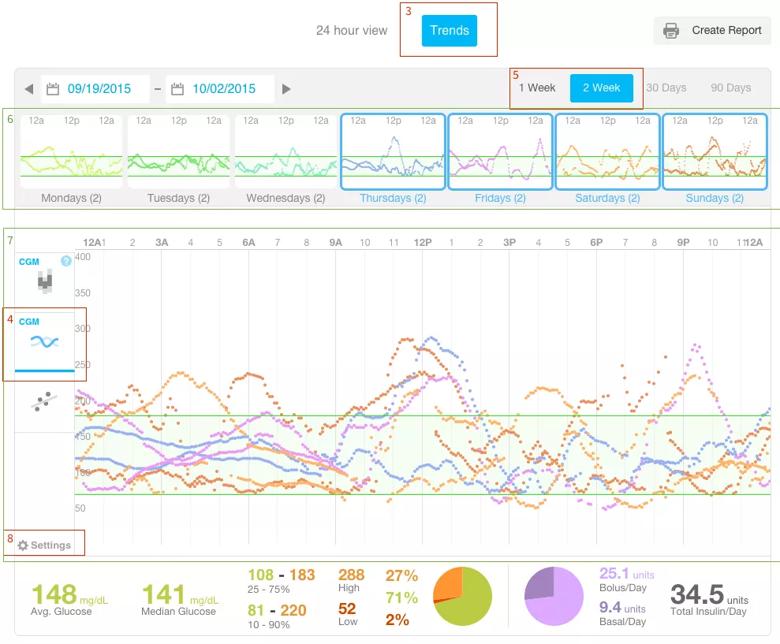
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5d012cbc-96ab-465e-8b68-391585fbccf3/20-HVI-1961367-glooko-screen-display-inset_png)
Figure. Example of a data report from the Glooko app. Image courtesy of Glooko (glooko.com/2015/10/dailytrends/).
Advertisement
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable