Metrics developed by physicians a way forward in healthcare

Cleveland Clinic urologists have developed a patient-centered, novel hospital quality scoring system that is predictive of mortality following radical cystectomy. Robert Abouassaly, MD, staff urologic oncologist at Cleveland Clinic’s Glickman Urological & Kidney Institute, and colleagues created the tool in response to a lack of validated quality scoring systems specifically tailored to bladder cancer surgery, one of the most complex and costly surgeries performed in all of urology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“As urologists, we often are subject to metrics that are created with little input from practicing physicians,” says Dr. Abouassaly. “They are often process related, with little impact on patient outcomes. Our metric brings urologic surgeons — the people actually delivering the care — into the conversation.”
The researchers published their results in The Journal of Urology in 2019 after presenting their study results at the American Urological Association’s 2018 Annual Meeting.
The researchers used the National Cancer Database to gather data on hospitals performing radical cystectomy from 2004 to 2014 across the U.S. for a total of 48,314 patients. The team constructed mixed effects models and indirect standardization to measure hospital performance across several different quality metrics. Then, they created a composite hospital quality score for radical cystectomy, which was subsequently shown to correlate with 30-day, 90-day and overall mortality.
After assessing the current landscape of quality measurement in radical cystectomy, the researchers analyzed seven quality indicators: positive margins, performance of lymph node dissection, unplanned readmissions within 30 days, the proportion of patients with muscle-invasive bladder cancer who received neoadjuvant chemotherapy, the proportion of patients who underwent continent diversion, postoperative length of stay and time from diagnosis to surgery. A Bladder Cancer Quality Score (BC-QS) was created based on the performance of lymph node dissection during radical cystectomy, rate of positive surgical margins and delivery of neoadjuvant chemotherapy for eligible patients before surgery.
Advertisement
The overall score was then correlated to patient mortality, with better BC-QS performance associated with lower 30-day, 90-day and overall mortality (adjusted OR 0.78, 95% CI 0.64-0.96; OR 0.84, 95% CI 0.72-0.97; HR 0.86, 95% CI 0.81-0.92, respectively). The study showed that patients undergoing surgery at high-scoring hospitals are less likely to die — both in the short and long term.
“The findings were quite clear,” says Dr. Abouassaly, “and while they need further validation, we encourage hospitals to adopt this metric for radical cystectomy.”
This physician-developed and validated metric demonstrates the possibility of creating and need for developing disease-specific, outcome-associated metrics that are relevant to patient care and outcomes as well as hospital performance.
Researchers hope that the creation and validation of the BC-QS demonstrates the value of physician-developed metrics to policy makers and payers. “As we move toward value-based purchasing models, practicing physicians must be engaged in developing these metrics, or we risk assessment for the sake of assessment,” says Dr. Abouassaly. “Our scoring system is an important step toward this goal.”
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
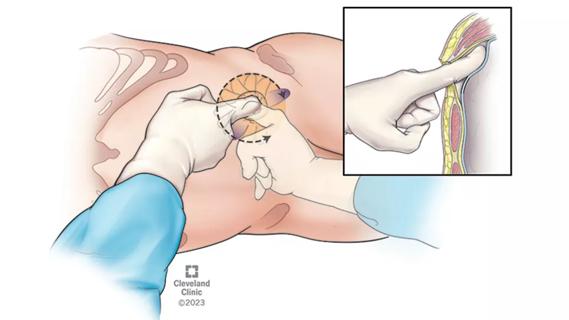
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
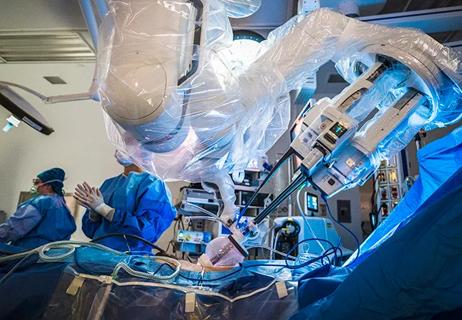
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients