Strategy also shortens procedural time
A strategy of high-power (50 W), short-duration (8-15 sec) radiofrequency ablation during pulmonary vein isolation (PVI) results in improved long-term PVI durability compared with conventional moderate-power (30-40 W), moderate-duration (20-30 sec) ablation in patients with atrial fibrillation (AF). The high-power, short-duration (HP-SD) approach also shortens the total ablation time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concludes a prospective study presented virtually this week during the Annual Scientific Sessions of the Heart Rhythm Society and published simultaneously in JACC: Clinical Electrophysiology.
“The incidence of AF recurrence after ablation is substantial, largely because of a high rate of electrical reconnection between the pulmonary vein and the left atrium,” says the study’s principal investigator, Elad Anter, MD, Associate Section Head of Cardiac Electrophysiology at Cleveland Clinic and Director of the Mark Josephson and Andy Wit Electrophysiology Research Laboratory.
To improve the clinical outcome of AF ablation and address the challenge of pulmonary vein reconnection, Dr. Anter’s translational research team has studied the biophysics of radiofrequency ablation using advanced computer simulations, ex vivo bench models and preclinical in vivo studies. They found that ablation at higher powers for shorter durations increases the desired effect on target tissue in immediate proximity to the catheter while reducing the undesired effect of ablation on neighboring structures, such as the esophagus and phrenic nerves. This strategy essentially shifts the classic energy distribution to increased heat by resistance and reduced heat by conduction (Figure).
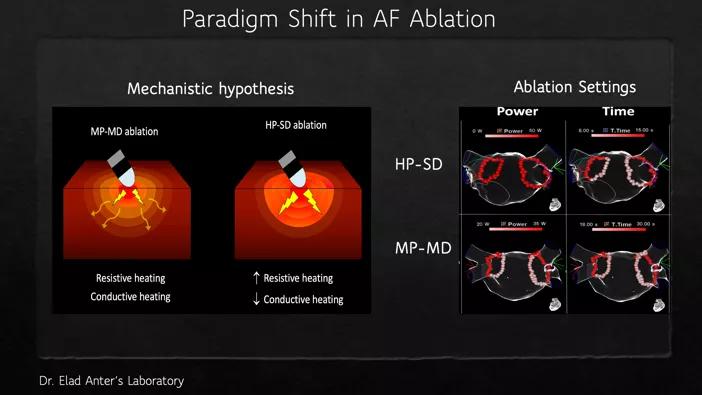
Figure. Visualization of key differences between high-power, short-duration (HP-SD) and moderate-power, moderate-duration (MP-MD) ablation strategies.
The team’s pivotal studies (JACC Clin Electrophysiol. 2018;4:467-479 and J Cardiovasc Electrophysiol.2018;29:1287-1296) have resulted in coining of the term HP-SD ablation and invigorated development of multiple technologies using HP-SD ablation strategies. “However, while this ablation concept has been intriguing, long-term outcome data had not been previously presented,” Dr. Anter observes.
Advertisement
He and his coinvestigators prospectively enrolled 112 patients with symptomatic paroxysmal or persistent AF to undergo AF ablation using the HP-SD ablation strategy — i.e., at a power of 50 W for 8 sec in the posterior wall and 15 sec in the ridge of the left pulmonary vein and the septal aspect of the right pulmonary vein. Results were compared with those of the preceding 112 patients who underwent ablation using a moderate-power, moderate-duration (MP-MD) strategy — i.e., 20 W in the posterior wall and 35-40 W in the in the ridge of the left pulmonary vein and the septal aspect of the right pulmonary vein applied for 20 to 30 sec using a similar catheter technology. Acute pulmonary vein (PV) reconnection was evaluated in all patients and chronic PV reconnection was examined in patients who required redo procedures (n = 18 for HP-SD; n = 23 for MP-MD).
Key findings included the following:
Advertisement
“Applying higher powers for shorter durations appears effective for PVI, as it reduced the incidence of PV reconnections and the overall procedural duration,” says Dr. Anter. “However, these data cannot be oversimplified. High power should be used diligently with careful attention to changes in impedance, temperature and electrograms. In particular, this strategy is effective for PVI and thin walls but not for thicker myocardium, which requires ablation at lower powers applied for longer durations to achieve transmurality without overheating the subendocardium.”
A key finding of the study, he adds, is the importance of catheter stability for lesion durability. “The accuracy of catheter stability required for creating durable ablation lesions is so high (< 1 motion) and is difficult to achieve when ablation is performed over relatively longer durations,” he says. “The advantage of the HP-SD ablation strategy is that this stringent stability is required only for a short period of time.”
Dr. Anter notes that catheter and generator technologies are now being refined to allow HP-SD ablation in an even safer and more effective fashion. This involves new catheter designs with larger surface areas, multiple temperature sensors and high-energy generators. Dr. Anter’s research team has been involved in the development of these technologies and their evaluation in humans.
“While no single ablation strategy is suited to all patients and all sites, electrophysiologists are starting to move toward ablation at higher power for shorter duration for improved long-term durability of pulmonary vein isolation,” observes Dr. Anter’s colleague, Oussama Wazni, MD, Section Head of Cardiac Electrophysiology at Cleveland Clinic. “The encouraging results from this study should accelerate that shift.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable