A call to use lung weight in assessing need for EVLP, transplant suitability

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/88c76899-8661-49ef-9be1-c1f0c8763cac/22-HVI-2903977_ex-vivo-lung-perfusion_650x450_jpg)
22-HVI-2903977_ex-vivo-lung-perfusion_650x450
High donor lung weight predicts lower transplant suitability after ex vivo lung perfusion (EVLP), higher rates of primary graft dysfunction 72 hours after transplant and longer intensive care unit/hospital stay compared with lower donor lung weight. So concludes a new single-center study of 365 human donor lungs that adjusted lung weights by donor height and correlated them with transplant outcomes. It was published online in the Journal of Heart and Lung Transplantation by Cleveland Clinic researchers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings suggest that donor lung weight — an easily obtained and objective measure that correlates with the more difficult-to-estimate extravascular lung water — is a good parameter for assessing transplant suitability and the need for EVLP.
“Consideration of donor lung weight can enhance decision-making regarding the need for EVLP at the donor hospital as well as during EVLP evaluation,” says the study’s senior and corresponding author, Kenneth McCurry, MD, Surgical Director of Lung and Heart/Lung Transplantation at Cleveland Clinic. “Our strategy for normalizing lung weight by donor height leads to better grading of extravascular lung water in donor lungs than simply using unstratified lung weight.”
Accumulation of extravascular lung water can occur in the donor before procurement and is exacerbated following ischemia reperfusion injury in the recipient after transplantation, leading to severe primary graft dysfunction and elevated mortality risk. Therefore, quantifying extravascular lung water in donor lungs prior to transplantation is an important consideration for whether the lungs should undergo EVLP, a process that can facilitate water removal and improve lung function to make a lung more suitable for transplantation. However, measurement of extravascular lung water is limited with traditional assessment methods.
No previous studies have examined the use of lung weight as a surrogate for extravascular lung water to predict suitability for transplantation. In a previous study published in the Journal of Surgical Research (2021;260:190-199), Dr. McCurry’s group found that among lungs rejected for transplantation, donor lung weight at procurement and change in lung weight during EVLP correlated with transplant suitability, as assessed by standard EVLP parameters. The current study was designed to extend these findings to evaluate the effect of donor lung weight with clinical outcomes after transplantation.
Advertisement
Between the launch of Cleveland Clinic’s clinical EVLP program in February 2016 and August 2020, 365 human donor lungs were evaluated for transplantation and had available lung weight data. The outcomes of these lungs were retrospectively analyzed in this study, revealing the following:
Lung weights, measured at time of procurement at the donor hospital and after EVLP, were adjusted by donor height and divided into four quartiles (the method of lung weight normalization is detailed in the article). Initial lung weight was significantly correlated with donor height (P < 0.0001, Figure) but not with donor weight, body surface area or body mass index.
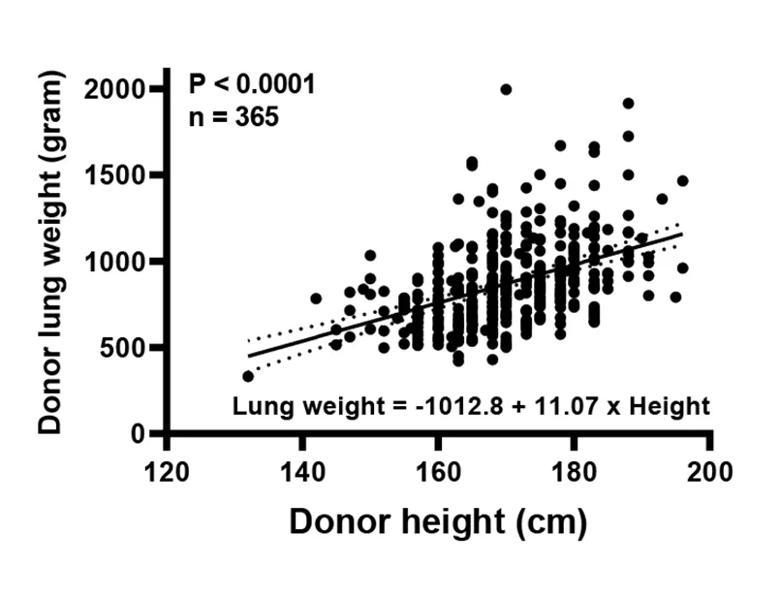
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/242c23f1-7799-4603-8595-3e02dd58a292/22-HVI-2903977-CQD-Inset-1_jpg)
Figure. A significant correlation was found between donor height and initial lung weight at the donor hospital.
Analysis of donor lung outcomes according to weight at procurement revealed the following notable findings:
Advertisement
The authors conclude that the study provides strong evidence that adjusted donor lung weight corresponds with extravascular lung water and correlates with suitability for transplant in both straight transplant cases and EVLP cases. “Whether measured at procurement or after EVLP, high adjusted lung weights were associated with worse clinical outcomes than lower lung weights,” notes the study’s first author, Toshihiro Okamoto, MD, PhD, Associate Director of Cleveland Clinic’s EVLP Program.
The authors recommend the following strategy based on height-adjusted lung weight at procurement:
“Nearly 90% of lungs that underwent EVLP gained weight after EVLP, by an average of 16%,” observes Dr. Okamoto. “This result is consistent with reports on the effects of acellular EVLP.”
The authors note that even though the heaviest lungs were the least likely to be transplantable after EVLP, there often is good reason to perfuse high-weight lungs, especially considering the scarcity of transplantable lungs.
“Our study indicates that donor lung weight might contribute to better grading of extravascular lung water, making it useful for helping to determine whether lungs can go straight to transplantation or should undergo EVLP first,” Dr. McCurry concludes. “Further study of long-term outcomes is needed to more fully evaluate this strategy.”
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable