Beyond the headlines of the STICH and INOVATE-HF trials
At first blush, the two big studies of interest to heart failure specialists presented at the American College of Cardiology’s annual meeting this spring seemed to have quite different story lines.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The international STICH trial confirmed its hypothesis that adding coronary artery bypass graft surgery (CABG) to medical therapy yields significant benefit over medical therapy alone with respect to all-cause mortality among patients with ischemic cardiomyopathy.
In contrast, the multicenter INOVATE-HF trial failed to show a reduction in the incidence of heart failure events or all-cause mortality with vagus nerve stimulation among patients with chronic heart failure and a reduced ejection fraction.
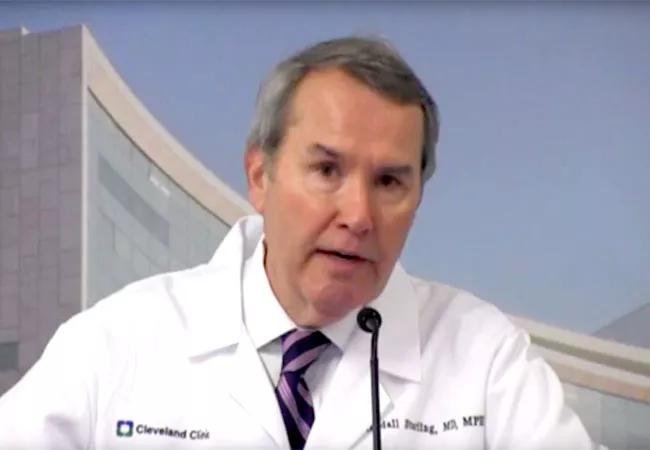
Yet in the pair of videos below, INOVATE-HF co-investigator and Cleveland Clinic heart failure specialist Randall Starling, MD, MPH, notes that there’s more to each study than first meets the eye.
In the first video, which focuses on STICH, Dr. Starling notes that the study leaves one key question — How does CABG compare with percutaneous coronary revascularization for patients with ischemic cardiomyopathy? — unanswered for now.
In the second video, which focuses on INOVATE-HF, Dr. Starling explains why vagal nerve stimulation still may hold promise in heart failure despite this study’s disappointing results.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable