EMR-integrated tool focuses on discharge preparation to avert readmissions

If heart failure (HF) readmissions are to be prevented, the time to make a difference is during in-hospital discharge preparation or transitions at discharge.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That was the hypothesis behind Cleveland Clinic’s Heart Failure Checklist when it was first conceived in 2011. The real-time electronic checklist — one of the first in the nation to be fully integrated into the electronic medical record (EMR) — has since borne out that hypothesis in two big ways.
First it enabled Cleveland Clinic to achieve its lowest-ever 30-day HF readmission rates — and to sustain those rates for three years and counting. And now it has helped Cleveland Clinic win the 2017 HIMSS Enterprise Davies Award from the Healthcare Information and Management Systems Society (HIMSS). The award, the highest honor from HIMSS and the only one granted to healthcare providers, recognizes outstanding achievement by an organization in using health information technology to substantially improve patient outcomes and value.
“The Heart Failure Checklist leverages analytics from the EMR and uses clinical decision support to ensure that every patient with HF is identified while in the hospital and then receives appropriate multidisciplinary care,” says Umesh Khot, MD, Vice Chair of Cardiovascular Medicine, who spearheaded the project.
“The checklist does this with real-time data inputs at the point of care that reflect the true multidisciplinary coordination of care involved in managing patients with HF,” adds Randall Starling, MD, MPH, Medical Director of Cleveland Clinic’s Kaufman Center for Heart Failure and part of the leadership team behind the project. “It ultimately leads to an electronic ‘hard stop’ in the EMR to ensure that all checklist items have been completed for the patient before discharge can proceed.”
Advertisement
The project was a long time coming, notes heart failure cardiologist Corinne Bott-Silverman, MD, another member of the project’s leadership team. “Programs to reduce HF readmissions at our organization had been attempted with little success, from discharge follow-up calls to telemonitoring and other approaches,” she explains. “After much data analysis, we found that preventable readmissions tend to occur early.”
That observation spurred the hypothesis that success in reducing HF readmissions would lie in interventions during patients’ hospital stay and in transition at discharge. “So we proposed an HF discharge checklist and corresponding in-hospital care metrics,” notes Dr. Khot.
The checklist was first developed in paper form and called for information on patient readiness for discharge to be supplied by nursing, pharmacy, nutrition care management, and the physician or advanced practice provider. The aim was to bring all discharge-relevant information together in one place for easy tracking.
The paper checklist was tested in a 12-week pilot study with two services on a heart failure unit. Patients managed with the checklist had a 14.6 percent 30-day readmission rate, which compared well with the 22.1 percent rate for HF controls managed without the checklist and the unit’s historical 25 percent readmission rate from the prior year. “Patients managed with the checklist had one of the lowest HF readmission levels we had seen,” says Dr. Starling. “These results grabbed our attention.”
Advertisement
The concept was further validated when readmissions for the unit’s patients spiked when checklist use was temporarily stopped after the pilot — and again when rates went back down to pilot levels when checklist use was resumed.
“We had proven the concept, but we needed to take it to a larger scale,” observes Dr. Khot. Yet the checklist’s paper format made that a huge challenge, as it required labor-intensive manual completion and had limited reporting and analysis capabilities.
So the project team created a governance structure to transition the HF discharge checklist from paper to electronic form and secured funding for contracted resources. They then identified the key roles from the paper checklist and where documentation for each would be discretely captured in the EMR for the electronic checklist. This was done by a multidisciplinary team — representing nursing, quality, IT, nutrition, pharmacy and care management – formed with the clinical leadership.
Key features of the resulting electronic checklist included:
Advertisement
After more than 13 months developing the paper checklist into its electronic version, the team was ready to take the electronic tool live in November 2014.
But implementation presented its own challenges. Chief among them was the fact that many frontline caregivers were not sufficiently aware of the checklist or the institutional priority that had been given to reducing HF readmissions. Manifestations included excessive use of the checklist on patients who didn’t need it, concern that checking boxes was being prioritized over care delivery, and refusal to use the checklist because of misunderstanding about the motivations behind it.
“We had focused too much on the technology at the expense of human factors,” observes IT project manager Tim Sobol, MS. “It became clear that we needed to educate frontline caregivers on why we were doing this and engage them in the process.”
So the team created a simple infographic explaining the “why, who and what” behind the checklist, with supporting details. This served as the centerpiece for a new round of education to support the checklist’s launch. “Our education emphasized that this was about ensuring care coordination across the various disciplines involved in HF care,” explains Kathleen Kravitz, a quality director with Cleveland Clinic’s Miller Family Heart & Vascular Institute. “We also stressed that readmission prevention is a process that starts at admission and informs all aspects of normal clinical care, not just the portion right before discharge.”
Advertisement
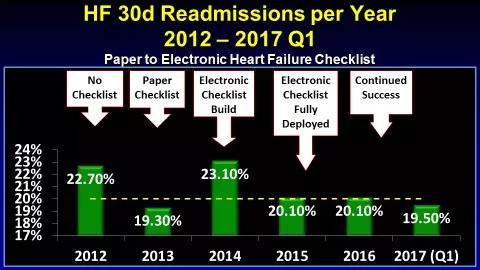
With this additional educational push, the checklist was embraced and implemented for more than 1,500 patients with HF over the first six months of rollout. As detailed in the graph below, 30-day HF readmission rates have been at or below the 20 percent target level for each year since introduction of the electronic checklist in late 2014.
Beyond the clear patient benefits from fewer readmissions, the checklist has already more than offset its contracted resource cost through reductions in CMS penalties for excess HF readmissions at Cleveland Clinic’s main campus hospital alone.
“The Heart Failure Checklist has been a technical and operational success, with 100 percent implementation across our Heart & Vascular Institute that’s now been in place for several years,” says Dr. Khot. “We’ve seen significant decreases in our readmissions locally and in public reporting, and there’s been a significant return on investment for the project.”
For other organizations considering a similar initiative, he offers two key pieces of advice:
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable