Optimal timing still questioned
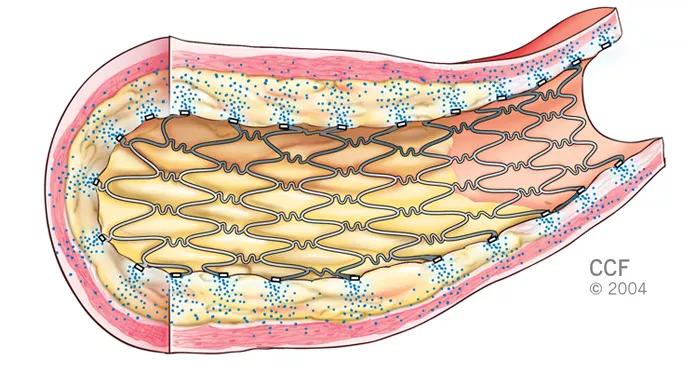
Multivessel percutaneous coronary intervention (PCI) is now recognized as a therapy option in patients with ST-elevation myocardial infarction (STEMI) following release of a focused guideline update from a group of leading cardiovascular medical societies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Previous clinical practice guidelines recommended against PCI of nonculprit artery stenoses at the time of primary PCI in hemodynamically stable patients with STEMI. But four randomized clinical trials have since suggested that the practice may be both beneficial and safe in properly selected patients. Based on these results, joint guidelines from the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA) and the Society for Cardiovascular Angiography and Interventions (SCAI) were changed to upgrade PCI in noninfarct arteries from a Class III “harm” to a Class IIb recommendation.
“Improvements in STEMI-related PCI pharmacology and techniques have increased the safety of multivessel PCI, both at the time of STEMI and in staged procedures, such that patients with high-grade lesions in large, nonculprit vessels should be considered for multivessel PCI,” says Stephen G. Ellis, MD, Director of Interventional Cardiology at Cleveland Clinic. “However, some data suggest this should be performed in a staged fashion rather than simultaneously, except in patients who are in cardiogenic shock.”
Dr. Ellis served on the writing committee that updated recommendations made in the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, and he was joined by his Cleveland Clinic electrophysiologist colleague Mina Chung, MD, who served on the committee that updated the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction.
Advertisement
The 2013 designation of multivessel PCI as a Class III “harm” recommendation was made when a composite of clinical trials, observational studies and meta-analyses comparing culprit artery–only PCI with multivessel PCI yielded conflicting results. However, comparisons in that effort were made difficult by differences in inclusion criteria, study protocols, timing of multivessel PCI, statistical heterogeneity and variable end points.
Safety concerns included increased risks for procedural complications, prolonged procedural time, contrast nephropathy and stent thrombosis. They also stemmed from findings from many of the observational studies and meta-analyses showing trends toward, or statistically significant increases in, worse outcomes with multivessel primary PCI.
At the time, PCI of noninfarct artery stenoses was considered only for spontaneous ischemia or high-risk findings on predischarge noninvasive testing. Staged PCI was not addressed.
Four clinical trials presented between 2013 and 2015 reversed this thinking:
All four studies evaluated multivessel PCI at the time of primary PCI or as a planned, staged procedure and found that fewer patients treated for multivessel disease met the composite end point of adverse cardiovascular events compared with patients who received PCI only on the culprit lesion.
Advertisement
“Although the data were not particularly strong, when added to extensive data from registries, the aggregate data suggest it’s best to treat the nonculprit lesion soon after discharge,” says Dr. Ellis.
More definitive information will come from the ongoing COMPLETE trial. This 3,900-patient global trial is comparing the effectiveness of complete vs. culprit-only revascularization of multivessel disease after primary PCI for STEMI. The study is powered to determine whether staged PCI revascularization of nonculprit lesions effectively reduces the incidence of death and MI.
Cleveland Clinic’s approach to multivessel PCI gradually evolved as the four clinical trials on which the guideline update was based were released, Dr. Ellis notes. “We have moved toward doing a better job of complete revascularization within the month after STEMI, but generally not at the time of STEMI, except when the patient is in cardiogenic shock,” he says.
He cautions that the guideline update should not be interpreted as endorsing the routine performance of multivessel PCI in all patients with STEMI and multivessel disease.
“Biochemical changes induced by STEMI — notably inflammation — cause nonculprit stenosis instability, but you have to use common sense,” Dr. Ellis says. “With an inferior STEMI, you could have a proximal left anterior descending coronary artery that is 95 percent blocked. In such a patient, leaving it without simultaneous multivessel PCI might be precarious. In a patient with a nonculprit third marginal artery that is 50 percent blocked, the situation would be much different.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable