A snapshot of a less-invasive alternative to open-heart repair
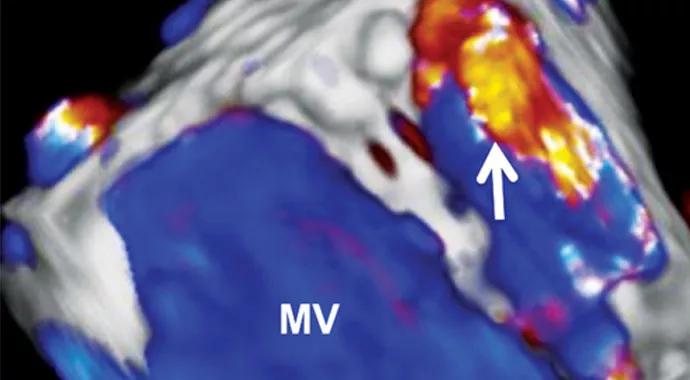
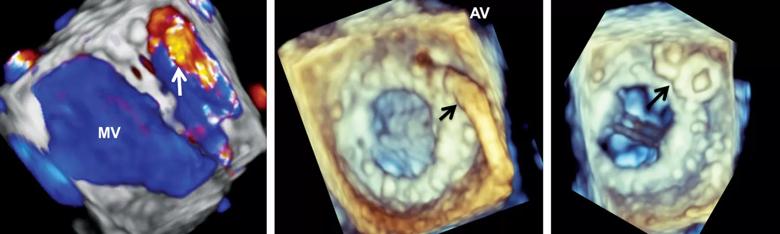
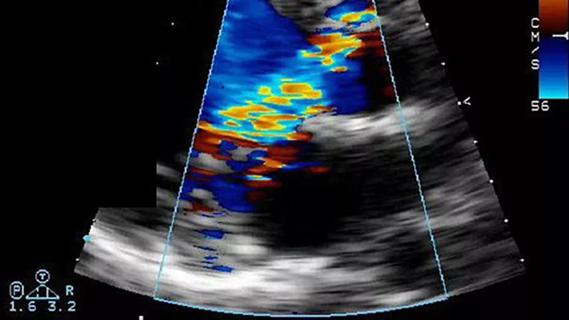
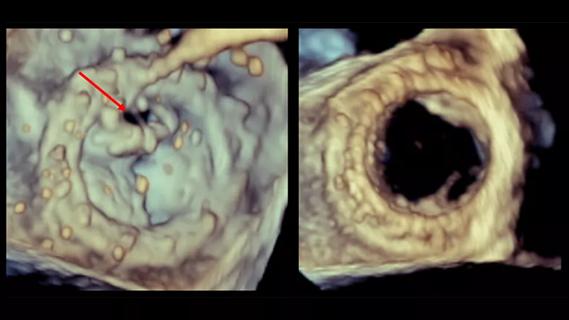
Images: Percutaneous closure of a paravalvular leak (PVL). Left: 3-D transesophageal echocardiogram (TEE) with color Doppler demonstrates a large anteromedial PVL (arrow). Middle: 3-D TEE with the delivery catheter in place (arrow). Right: 3-D TEE with two Amplatzer Vascular Plugs II in place (arrow). AV = aortic valve; MV = mitral valve. Reproduced from Chenier M, Tuzcu EM, Kapadia SR, Krishnaswamy A. Intervent Cardiol. 2013;5(3):335-344.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patients with prosthetic heart valves who present with symptoms of heart failure or hemolytic anemia may suffer from paravalvular regurgitation, also known as paravalvular leak (PVL).
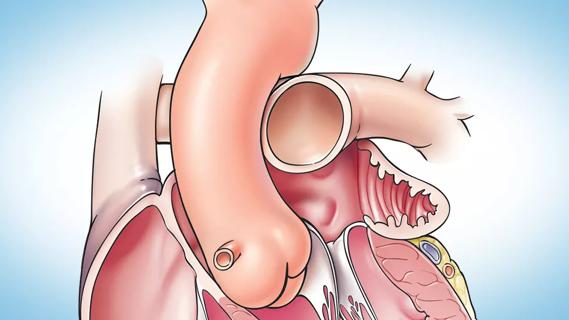
Traditionally, PVL has been repaired with repeat open-heart surgery, which can pose greater risk than a first time operation and carries a risk of recurrent PVL. In recent years, experienced interventional cardiologists have achieved excellent results with percutaneous closure of PVL. Outcomes at Cleveland Clinic and other well-equipped centers suggest that this structural intervention has a promising future.
PVL is the result of a space between the native cardiac tissue and the prosthetic valve. It occurs in about 2 to 12 percent of patients with bioprosthetic or mechanical valves, and more often in the mitral than the aortic position. PVL in the tricuspid position is rarer still, but it can occur.
Risk factors for developing PVL include (among others) multiple valve replacements in the same position, severe calcification of the valve annulus and surgery for endocarditis.
Recognition of PVL usually starts with suspicion arising from the clinical history. The diagnosis is then made by echocardiography. Often, transthoracic echocardiography is limited by “shadowing” around a prosthetic valve, and transesophageal echocardiography (TEE) must be performed to confirm the diagnosis.
Advanced imaging is critical to planning and performing the procedure. Operators may be guided by 2-D and 3-D TEE, intracardiac echocardiography, fluoroscopy/angiography and, recently, combined CT and fluoroscopy.
Advertisement
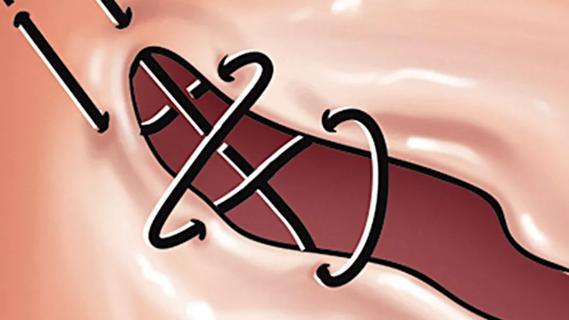
Leaks are repaired by placing one or more nitinol plugs in the defect, much like stuffing a cotton ball in the top of a medicine bottle. There are currently no devices specifically designed to treat PVL. Instead, operators use one or another vascular or septal occluder based on the leak’s size and shape. Choice of device is guided by preprocedural imaging and intraprocedural monitoring.
Percutaneous closure of a paravalvular mitral leak is performed one of three typical ways:
Aortic valve procedures are generally done via the femoral artery.
Aside from procedures for which apical access is necessary, percutaneous PVL closure at Cleveland Clinic is performed using local anesthesia and conscious sedation, not general anesthesia, and without endotracheal intubation.
Small reports and large series have been published over the past 20 years showing that percutaneous PVL closure is safe and efficacious. Most patients enjoy freedom from significant heart failure symptoms, blood transfusions due to hemolysis or need for repeat open-heart surgery.
The procedure requires a highly skilled and experienced team of interventional cardiologists, imaging cardiologists, and catheterization lab technicians and nurses with access to specialized equipment and advanced imaging modalities.
Advertisement
Performed carefully, percutaneous PVL closure provides an effective but less-invasive alternative to repeat open-heart surgery for a number of patients suffering from this condition.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
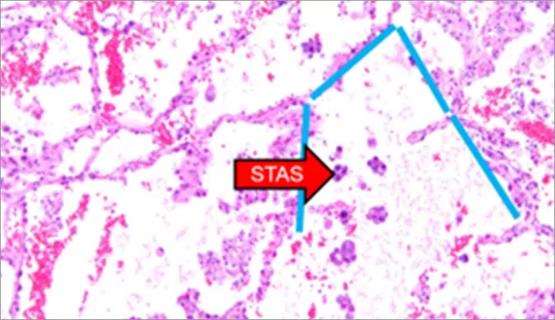
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable