An option for difficult-to-treat chronic knee pain
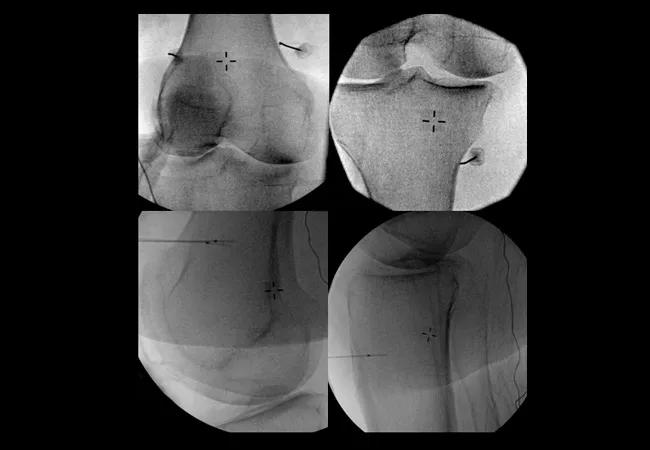
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8627fa69-8b39-4a49-a33b-aa74b9fa32fe/16-ORT-1510-Schaefer_Hero-Image_650x450pxl_jpg)
16-ORT-1510-Schaefer_Hero-Image_650x450pxl
By Michael Schaefer, MD, and Robert Bolash, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic knee pain is often a challenging condition to treat. Pharmacologic interventions commonly fail to provide adequate relief and can be limited by adverse effects. Corticosteroid injections provide only temporary relief, while hyaluronate injections are expensive and controversial. Newer “regenerative” injection treatments such as stem cells and platelet-rich plasma are still considered experimental and are often not covered by insurance. Surgical interventions for joint preservation are limited, and total joint replacement is often not an option for young or obese patients. Even after arthroplasty, unremitting knee pain continues to afflict some patients.
Radiofrequency ablation for genicular nerves (GNRFA) is a relatively new and lesser-known treatment option that is proving effective for certain patients. A randomized controlled trial demonstrated significant improvement with GNRFA throughout the 12-week follow-up period. At Cleveland Clinic, we consider patients for GNRFA who have failed or are excluded from other treatment modalities. The process begins with a diagnostic genicular nerve block.
Genicular nerve blocks can be performed under fluoroscopic or ultrasound guidance. Nerves are targeted adjacent to the periosteum on the medial aspect of the tibia, and at both the medial and lateral aspects of the femur at the junctions of the shaft and the epicondyle.
Under fluoroscopic guidance, we approach the target by introducing a spinal needle from either an anteroposterior or lateral entry point with the final position residing adjacent to the bone. After negative aspiration, some physicians elect to administer contrast to exclude vascular uptake, avoiding a false negative result. To conclude the procedure, 2 mL of local anesthetic is deposited on each of the superolateral, superomedial and inferomedial genicular nerves.
Advertisement
While GNRFA performed under fluoroscopic-guided requires a procedure room, the ultrasound-guided procedure can be performed conveniently in the outpatient clinic setting without radiation exposure. In addition, two recent studies suggest ultrasound guidance improves accuracy of the diagnostic block by localizing arteries and soft tissues adjacent to the nerves. Again, all three genicular nerves are routinely injected – the superomedial, superolateral and inferomedial branches. Other branches have been reported to innervate the knee, but they are not suspected to carry as much nociceptive output from the joint, so injecting them may be less effective. In patients who report pain only on the medial side of the knee, the physician may choose to inject only the medial-sided nerves.
If the diagnostic injection produces at least 50 percent pain relief on a numeric rating score reduction, the patient is deemed a candidate for GNRFA. Exclusions include systemic or local infection and electrical devices implanted in the region of the radiofrequency ablation. Additional vigilance is required in the presence of anatomic deformities or implantable cardiac rhythm devices when considering GNRFA because of the potential for a defibrillator to interpret radiofrequency as a shockable dysrhythmia. GNRFA can successfully be performed with arthroplasty or with other orthopaedic hardware in place.
The GNRFA procedure is typically performed with local anesthetic, although moderate IV sedation may be offered. Either ultrasound or fluoroscopic guidance may be used. Following local anesthetic infiltration, a radiofrequency cannula is guided in proximity to the locations of each nerve. Sensory stimulation can be used to confirm accurate placement. Motor stimulation is also performed to ensure the absence of adjacent motor fibers.
Advertisement
After positive confirmation of sensory placement and negative motor testing, 2 mL of 2 percent lidocaine is administered adjacent to the nerve to mitigate pain associated with radiofrequency lesioning. Radiofrequency ablation is performed at a temperature of 70 C for 90 seconds.
Postprocedurally, patients remain ambulatory and often return to work on the subsequent day. A few days of localized soreness is expected following the procedure with typical final results realized within one week.
While Choi showed that relief continued for 12 weeks, in our practice, we have seen many patients sustain even lengthier analgesia, at times approaching a year. The GNRFA may be repeated if symptoms return.
GNRFA is a suitable management option for a subset of patients with inadequate response to more conservative modalities and even for those with postsurgical refractory knee pain.
Dr. Schaefer is Director of Musculoskeletal Rehabilitation at Cleveland Clinic.
Dr. Bolash is an anesthesiologist and interventional pain management specialist in the departments of Pain Management and Evidence Based Pain Research.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions