Intensive program has multiple lasting benefits

For the nearly 300 patients with disabling chronic pain who enroll annually in Cleveland Clinic’s Chronic Pain Rehabilitation Program (CPRP), return to a normal level of function is management priority No. 1.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our emphasis is on functional restoration rather than on curing the pain itself,” explains CPRP Medical Director Xavier Jimenez, MD. “Function is more determined by factors that patients can learn to successfully control, such as general health, fitness and psychological well-being.”
To that end, the CPRP offers individuals who have undergone numerous unsuccessful attempts to stop chronic pain an intensive program of multimodal interventions including:
Patients participate in the program — one of the first of its kind in the nation, dating back to 1979 — from 7:30 a.m. to 5 p.m., Monday through Friday, typically for three to four weeks.
Data and outcomes for the 281 patients who enrolled in the program in 2015 — the latest year for which complete data are available — are typical for the CPRP overall and are summarized here. The 2015 patient sample was two-thirds female, with a mean age of 47.5 years (± 13.6 SD).
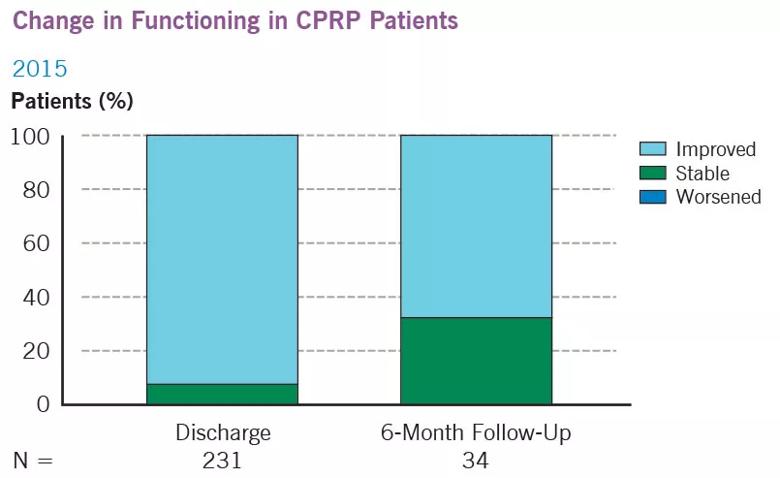
Outcomes data show that the program is highly successful in meeting its primary goal of functional improvement (see table below). Among the 237 patients who completed the program in 2015 (84 percent of enrollees), 97 percent provided information on their function at discharge.
Of these, 93 percent reported improved function at discharge as measured by the Pain Disability Index (improved function was defined as a decrease of at least 9 points on the 70-point scale). The remaining 7 percent had stable function, defined as a less than 9-point change in score. No patients had clinically significant deterioration.
Advertisement
Among all 34 patients who provided six-month follow-up information, function continued to be either improved (68 percent) or stable (32 percent).
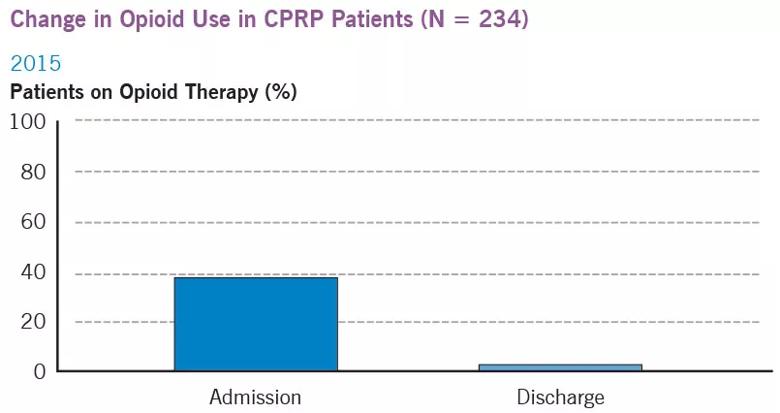
The use of opioid medications for chronic pain have been called into question by pain control experts as the dangers of dependence, tolerance and addiction have become increasingly well recognized.
“We expect that virtually all patients will be off opioid medications by the time of discharge,” says Dr. Jimenez. “We have a humane and safe program to accomplish this.”
The 2015 outcome data corroborate this goal. Among the 234 patients completing the program with complete data on opioid use, 87 (37 percent) were on chronic opioid therapy at the time of program admission (mean daily morphine milligram equivalence dosage, 48.53 + 108.75). By the time of discharge, 81 of these patients (93 percent) were fully weaned. Six-month follow-up data were available for 21 patients, all of whom were still opioid-free.
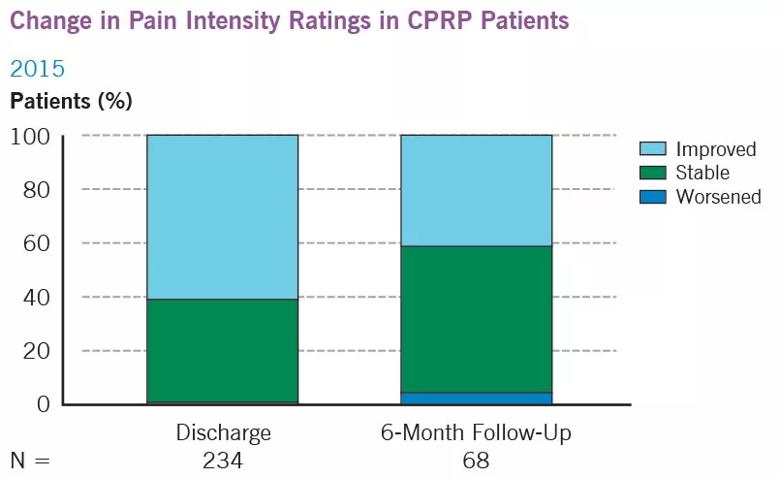
Although not a primary stated goal of the CPRP, outcomes snapshots revealed that pain lessened for many at discharge and six months later.
Program participants were evaluated for pain levels using a 10-point scale (0 = no pain, 10 = worst possible pain), with clinically significant change defined as at least a 2.5-point change. Of the 237 patients completing the program, 234 provided admission and discharge information about their pain intensity, with 60.7 percent showing improvement and 38.9 percent reporting stable pain (one patient reported worsening pain).
Advertisement
Six-month follow-up data were available for 68 participants, with 41 percent showing improvement, 54 percent having stable pain intensity and less than 5 percent reporting worsened pain.
Depression and anxiety were also assessed, using the Depression Anxiety Stress Scale (DASS-21): 234 patients provided information at discharge and 41 at six-month follow-up. Patients whose change in score was less than 7 points were deemed stable. As can be seen from the table below, depression and anxiety symptoms improved or remained stable for the vast majority of patients at discharge compared with baseline, with most patients maintaining these gains at six-month follow-up.
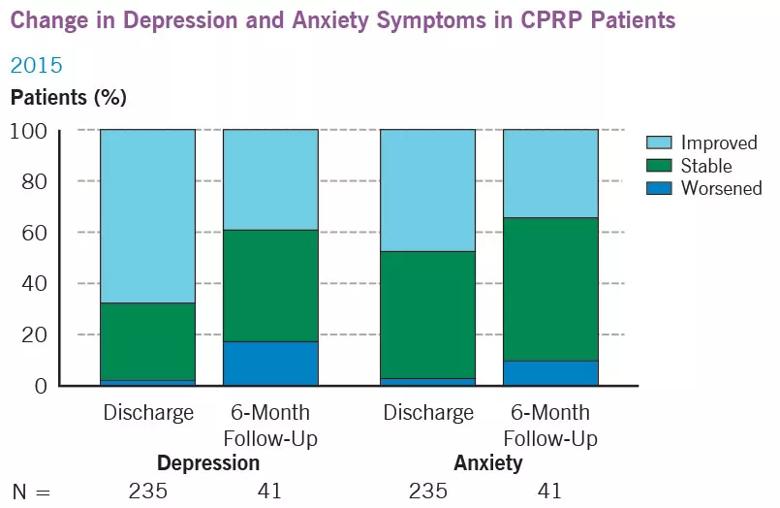
Dr. Jimenez reiterates that the program emphasizes rehabilitation of patients to their maximum level of function: “All other gains — lessening of pain, depression and anxiety — are a bonus,” he says.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade