Study finds similar short-term outcomes despite differing presentations
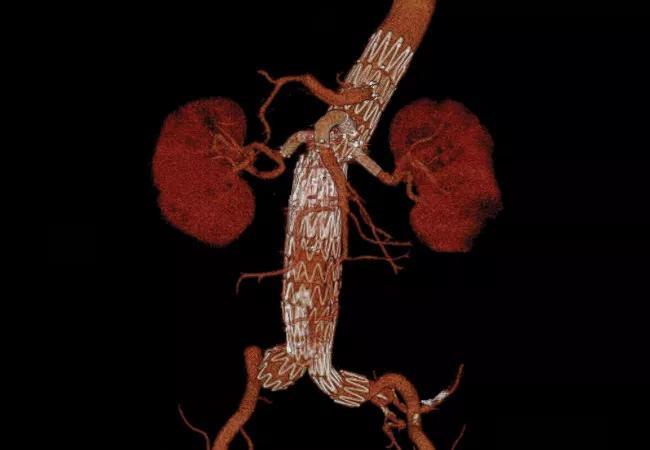
As rates of failed endovascular aortic aneurysm repair (EVAR) rise, so does the need to better understand optimal methods of managing failed EVAR cases. Results of a large Cleveland Clinic analysis presented at the Society for Vascular Surgery’s 2017 Vascular Annual Meeting show that open and endovascular management methods are comparable in 30-day reintervention and mortality rates but tend to be used for different modes of EVAR failure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cleveland Clinic is seeing more and more patients who present with failed standard EVAR that we need to repair,” explained the study’s principal investigator, Matthew Eagleton, MD, of Cleveland Clinic’s Department of Vascular Surgery. “We’ve traditionally taken two completely different approaches to these cases, so we wanted to compare them to assess any differences between the two modes of therapy.”
The investigation was a retrospective analysis of 247 patients treated for failed EVAR at Cleveland Clinic from 1999 to 2016. Patients underwent either open surgical explantation (n = 162) or endovascular therapy with fenestrated-branched EVAR (FB EVAR) (n = 85), which was performed under a physician-sponsored investigational device exemption (IDE).
Various patient characteristics — demographics, clinical presentation, failure etiology, perioperative management — and short-term rates of reintervention and mortality were statistically compared between the two methods.
The overall sample was 87 percent male and had a mean age of 75 years (range, 50-93).
There were no significant differences between the explant group and the FB EVAR group in graft manufacturer for the primary EVAR, and endoleak was the most common reason for primary EVAR failure in both groups. Beyond that, the groups differed significantly in EVAR failure etiology and other key clinical factors, as follows:
In the FB EVAR group, the mean time from primary EVAR was longer, and failure of the primary EVAR was more likely to involve a type I endoleak and to include graft migration and neck degeneration/disease progression.
Advertisement
In the explant group, a higher proportion of patients required urgent/emergent surgery, aortic rupture was more prevalent, and the presence of primary EVAR graft infection was more common (17 percent vs. 0 percent in FB EVAR group). Additionally, failure of the primary EVAR in the explant group was more likely to involve a type II endoleak and to involve aneurysm enlargement.
Analysis of outcomes showed no significant differences between the two management methods:
The absence of significant differences in reintervention or mortality rates was not altered by subset analysis excluding emergent/compassionate-use cases and cases involving infections and ruptures.
“These results suggest that explants and fenestrated-branched EVAR are both useful and necessary options for treating patients with failed EVAR,” said Dr. Eagleton. “Different modes of primary EVAR failure appear to point to a preferred method of treatment, but short-term outcomes are comparable between these options.”
He noted that the findings are reassuring in that they suggest “there’s no reason to hesitate in undertaking FB EVAR in a high-risk patient who’s not likely to tolerate open surgery, while in healthier patients we can safely proceed with open repair and expect very good long-term survival.”
He added that while future studies would be helpful to better match specific modes of failure with the best treatment option and to assess longer-term outcomes, “in the meantime surgeons should individualize management of EVAR failure according to the patient’s presentation and the resources available.”
Advertisement
In a second presentation at the 2017 Vascular Annual Meeting, Dr. Eagleton and colleagues reported results showing that choice of balloon-expandable covered stent does not appear to affect branch durability after FB EVAR.
“The ideal mating stent for target vessel revascularization in FB EVAR of the juxtarenal (JRAA) and thoracoabdominal (TAAA) aortic aneurysms is not known,” said Dr. Eagleton in explaining the study’s rationale.
To shed light on this question, he colleagues and analyzed clinical data from 918 patients undergoing FB EVAR for JRAA/TAAA at Cleveland Clinic in a prospective physician-sponsored IDE trial from 2003 to 2015. Among these patients, 1,604 renal arteries and 714 superior mesenteric arteries were mated with reinforcing fenestrations using either JOSTENT (Abbott Vascular) or iCAST™ (Atrium Medical) balloon-expandable covered stents.
They found that stent type did not significantly impact primary patency at five years, time to first reintervention or incidence of type III endoleaks. “Although we observed that selective distal self-expanding stent placement in vulnerable renal arteries may offer a safeguard against a primary occlusive event, overall results showed that stent design does not affect primary patency and overall reintervention rates in fenestrated endograft repair of aortic aneurysms,” Dr. Eagleton concluded.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable