Case studies add to our understanding of this rare condition
By Soumya Chatterjee, MD, MS, FRCP
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
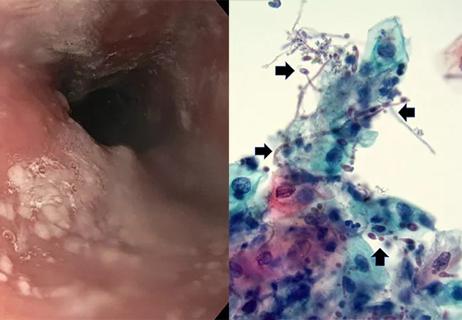
Two female patients with anti-polymyositis (PM)-scleroderma (Scl) antibody-associated systemic sclerosis developed progressive proximal myopathy. Both patients had profound muscle weakness that was refractory to treatment with glucocorticoids with or without other oral immunosuppressive agents. In this report, we describe these two cases of anti-PM-Scl antibody-associated scleromyositis in which a muscle biopsy unexpectedly showed features of sporadic inclusion body myositis (sIBM).1
Patient 1 (P1) is a 54-year-old female who presented with complaints of polyarthralgia, profound muscle weakness, Raynaud’s phenomenon and dysphagia. Her symptoms had insidious onset when she was 37 years old. Examination reveals mild sclerodactyly, but no proximal skin tightness. She had an ulcer on her right thumb with underlying calcinosis. Nailfold capillaroscopy revealed a paucity of capillaries, but no dilated loops or hemorrhages. P1 also had a profound proximal weakness, with some distal muscle weakness. Although she did not have the characteristic flexion contractures of systemic sclerosis, she was unable to make a fist, which we attribute to finger flexor weakness. Tendon reflexes and sensory exams were normal, as were exams of the cardiovascular, respiratory and gastrointestinal systems. Relevant laboratory studies include normal muscle enzymes, a positive antinuclear antibody and a positive anti-PM-Scl antibody. Left quadriceps muscle biopsy revealed endomysial inflammation and rimmed vacuoles in scattered muscle fibers, which is consistent with a diagnosis of sIBM.
Advertisement
When P1’s muscle weakness did not improve on high-dose glucocorticoids, she refused a trial of methotrexate or azathioprine. However, she did start high-dose monthly intravenous immunoglobulin infusions at 2 g/Kg/Cycle. In the four years since P1 notes stabilization of muscle weakness, but the severe proximal myopathy of her lower extremities and weakness in finger flexors and shoulder abductors persists.
Patient 2 (P2) is a 44-year-old female with a 9-month history of symmetrical polyarthritis, proximal muscle weakness, Raynaud’s phenomenon and dysphagia with frequent episodes of choking. The patient was initially seen by rheumatology at 37 years old. Exam reveals sclerodactyly without proximal skin tightness; an erythematous, dry and scaly rash over the extensor aspects of the bilateral metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints; and cuticular overgrowth with periungual erythema and telangiectasis and mechanic’s hands. Nailfold capillaroscopy revealed dilated loops, dropouts and hemorrhages. P2 had clinical synovitis of bilateral MCP and PIP joints, knees and ankles. Additionally, she had severe proximal and some distal muscle weakness. Weakness in her finger flexors, especially on her right side, led to an inability to make a fist. Tendon reflexes and sensory exams were normal, as were exams of the cardiovascular, respiratory and gastrointestinal systems. Notable laboratory results include elevated muscle enzymes and positive serologies (rheumatoid factor, anti-CCP antibody, ANA and anti-PM-Scl antibody).
Advertisement
P2 was diagnosed with seropositive rheumatoid arthritis (for which she was treated with oral methotrexate 20 mg weekly and six-monthly cycles of rituximab, each cycle included two 1,000 mg intravenous infusions two weeks apart) and sclero-dermatomyositis (for which she was treated with high-dose oral prednisone and monthly high-dose IVIG infusions). Over several months, her RA synovitis and dermatomyositis rash improved; however, her proximal and distal muscle weakness continued to progress. A left quadriceps muscle biopsy revealed focal endomysial chronic inflammation and rimmed vacuoles, suggestive of sIBM.
<p>Asymmetric weakness of deep finger flexors (left > right) in P1.</p>


<p>Hand radiographs in P1 showing calcinosis cutis.</p>

<p>Cuticular overgrowth with periungual erythema and nailfold capillary abnormalities in P2.</p>


<p>Weakness of the deep flexors of right index finger in P2</p>



Slide 1/8
In our two cases, a muscle biopsy was only considered necessary because of the treatment-refractory nature of their muscle disease. Similar to classic sIBM, both patients had quadriceps and finger flexor weakness, asymmetric muscle weakness and either normal or only modest elevation of muscle enzymes. Consistent with the previous two cases reported in the literature,2,3 the myositis in these patients was refractory to high-dose glucocorticoid therapy, with or without concurrent use of methotrexate or azathioprine. In anti-PM-Scl antibody-associated scleromyositis, the presence of rimmed vacuoles may indicate an acquired myositis that is distinct from classic sIBM, and some of these patients may respond more favorably to immunosuppressive therapy.
Advertisement
Our study indicates that, when anti-PM-Scl antibody-associated scleromyositis is treatment-refractory and involves distal muscles, it is prudent to obtain a muscle biopsy to ensure that the myositis is not due to sIBM rather than recalcitrant polymyositis or dermatomyositis. However, we have to keep in mind that rimmed vacuoles may sometimes be missed due to a sampling error. In the future, along with the anti-cN1A antibody, it may be appropriate to order an anti-PM-Scl antibody, especially in relatively younger sIBM patients with clinical characteristics suggestive of concomitant systemic sclerosis.
Advertisement
Advertisement

Treatment strategies require understanding of pathomechanisms

Education, prevention strategies and monitoring serves this at-risk group
Treatment for scleroderma can sometimes cause esophageal symptoms

Lupus Clinic providers collaborate to advance treatment and understanding

Older Psoriasis Patients May Experience Quicker Transition

Cleveland Clinic’s Rheumatic Lung Disease program treats patients with complex conditions

Symptoms complement one another

E-coaching program is tailored for those with the disease