In search of a useful diagnostic tool
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/59b3c746-62f4-41ba-8966-75aec620f49f/16-ORT-2501-Iannotti-Hero-Image-650x450pxl_jpg)
16-ort-2501-iannotti-hero-image-650x450pxl
By Joseph P. Iannotti, MD, PhD and Eric Ricchetti, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With the number of shoulder arthroplasties expected to quadruple in the coming years, the incidence of periprosthetic joint infection (PJI) of the shoulder is of great concern to orthopaedic surgeons.
This serious complication of shoulder replacement surgery is associated with poor outcomes, technically difficult revision surgery and increased costs. Accurate diagnosis is crucial to making decisions about treatment, including the decision to proceed with a one- or two-stage revision.
PJI of the shoulder often presents a diagnostic challenge due to the non-specific clinical presentation and indolent nature of the common infecting organisms, including Propionibacterium acnes (P. acnes) and coagulase-negative Staphylococcus species (CNSS). Patients frequently present only with symptoms of pain and stiffness in the shoulder, without other signs of infection.
In addition, standard diagnostic testing, effective in identifying knee and hip PJI, is far less effective in identifying shoulder infection. Serum erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) show sensitivities in the 80-90 percent range for PJI in the hip and knee, compared to less than 50 percent in the shoulder.
Preoperative synovial fluid aspiration is an important diagnostic test for shoulder PJI, as it provides the opportunity to diagnose infection prior to revision surgery. However, obtaining an adequate fluid sample for testing from the shoulder can be more challenging because of the decreased synovial fluid volumes that are present relative to the hip and knee. Due to this increased difficulty in aspirating the shoulder, limited data is available on its efficacy in diagnosis of shoulder PJI. Our group’s recent study sought to determine the rate of successful preoperative synovial fluid aspiration and its effectiveness in diagnosis of PJI in patients undergoing revision shoulder arthroplasty.
Advertisement
Our review included 202 cases evaluated for painful shoulder arthroplasty at Cleveland Clinic between January 2009 and February 2015. In 110 cases, a preoperative fluid aspiration was obtained and sent for culture, and 97 of these cases went on to revision arthroplasty surgery. Mean age at the time of surgery was 63.2 years (range, 29-89). We identified all cases of attempted preoperative aspiration to determine the incidence of successful and unsuccessful aspiration. Preoperative synovial fluid culture results were then compared to culture results at the time of revision surgery to determine the efficacy of preoperative synovial fluid aspiration for diagnosis of shoulder PJI.
Aspiration was attempted preoperatively in 137 of the 202 cases (68 percent), and a fluid sample was obtained and sent for culture in 110 of the 137 cases (80 percent). Of the 137 cases, 27 resulted in a dry tap (20 percent). Samples were culture positive in 18 percent of cases (20 of 110), with P. acnes the most commonly isolated organism (11 of 20, 55 percent). Of the cases in which a preoperative aspirate was obtained, 97 proceeded to revision surgery, including 20 with a positive and 77 with a negative preoperative aspirate culture.
Of those who underwent revision surgery, 59 percent (57 of 97) grew positive intraoperative tissue cultures, with P. acnes the most commonly isolated organism (43 of 57, 75 percent). Of the cases with positive preoperative cultures, 16 out of 20 (80 percent) grew positive intraoperative cultures, and the same organism was isolated in 15 of 16 cases. Of the 77 cases with negative preoperative cultures, 41 (53 percent) grew positive intraoperative cultures.
Advertisement
Sensitivity for preoperative aspiration in predicting infection was 26.3 percent and specificity was 87.5 percent, with positive and negative likelihood ratios of 2.11 (0.83, 5.32) and 0.84 (0.69, 1.02), respectively. Preoperative aspiration had a 75 percent positive predictive value and a 45.5 percent negative predictive value.
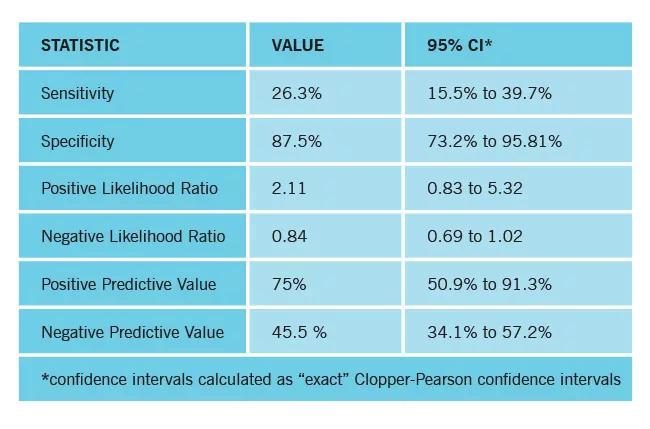
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/86838cfe-abcb-45d1-94d3-532e118b8b72/16-ORT-2501-Iannotti-Inset-Image-650pxl-width_jpg)
Diagnostic test characteristics for preoperative synovial fluid aspiration as a predictor of shoulder PJI using a definition of PJI based on Musculoskeletal Infection Society criteria, with two or more positive intraoperative cultures of the same organism representing infection.
Seventy-five percent (15 of 20) of patients with positive preoperative aspirates had more than 50 percent of their intraoperative cultures turn positive (average percent positive = 70) compared to 34 percent (26 of 77) in those cases with negative preoperative aspirates (average percent positive = 36) (p = 0.002).
In this study, we found that obtaining a preoperative aspiration sample for analysis was possible in the majority of patients (80 percent successful aspiration), and a culture positive sample was highly specific (87.5 percent) for the diagnosis of shoulder PJI. Having a positive preoperative culture was predictive of obtaining a positive intraoperative culture, with the same organism being identified 94 percent of the time, and was significantly associated with having more than 50 percent positive intraoperative cultures.
The timing of diagnosis of PJI can be important in determining management of this complex complication. When PJI is identified prior to or at the time of revision surgery, it can significantly impact treatment decision-making.
Advertisement
Dr. Iannotti (iannotj@ccf.org; 216.445.515) is Chair of the Orthopaedic and Rheumatologic Institute.
Dr. Ricchetti (ricchee@ccf.org; 216.445.6915) is staff in the Department of Orthopaedic Surgery.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions