Other factors explain diabetic patients’ poorer outcomes after bypass
A study presented at ACC.16, the American College of Cardiology’s 65th Annual Scientific Session, has challenged suspicions that diabetes affects long-term graft patency after coronary artery bypass graft surgery (CABG). The large retrospective analysis, drawing on nearly four decades of CABG cases at Cleveland Clinic, found long-term graft patency to be almost identical in patients with and without diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We had hypothesized that because diabetic patients have more severe stenosis in their coronary arteries, the disease in their bypass grafts would also be more severe than in nondiabetic patients, and this would result in worse bypass graft patency,” says primary investigator Joseph F. Sabik III, MD, Chairman of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “But this was not the case. Our findings suggest that worse outcomes after coronary surgery in diabetic patients are likely not related to lower graft patency and could be due in part to diabetic patients having more comorbidities, as well as progressive disease that leads to many complications.”
Dr. Sabik and colleagues tapped the breadth of Cleveland Clinic’s extensive Cardiovascular Information Registry to identify 57,961 patients who had undergone primary isolated CABG from 1972 through 2010. Patients were included in the analysis if they met the following criteria:
Of the 11,519 CABG patients who met these requirements, 1,372 had diabetes and 10,147 did not have diabetes. A total of 7,903 internal thoracic artery (ITA) grafts and 20,066 saphenous vein (SV) grafts were studied in these patients.
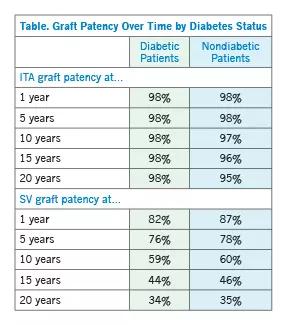
When outcomes at 1, 5, 10, 15 and 20 years were compared (Table), the results revealed a striking similarity in patency and stenosis patterns, with ITA grafts having excellent patency in both diabetic and nondiabetic patients whereas the patency of SV grafts decreased over time at comparable rates in both groups.
Advertisement
Because much of the long-term effectiveness of CABG depends on graft patency, the above findings suggest CABG should be as effective in diabetic patients as in nondiabetic patients. Yet mortality after CABG is much higher in the former group. Dr. Sabik believes this is likely due to noncardiac causes.
“It’s clear diabetic patients have more comorbidities and present with more problems at the time of surgery,” he says, citing findings of the Bypass Angioplasty Revascularization Investigation. That study, which compared cause of death in diabetic and nondiabetic patients at five years after CABG, found that while cardiac mortality was similar (5.8 percent in diabetic patients vs. 4.7 percent in nondiabetic patients), noncardiac mortality was much higher in diabetic patients (13.3 percent) than in their nondiabetic counterparts (5.6 percent).
Similarly, a 2015 study (J Thorac Cardiovasc Surg. 2015 Aug;150[2]:304-2.e2) led by Dr. Sabik drawing on the same Cleveland Clinic Cardiovascular Information Registry used in the current study revealed inferior post-CABG outcomes in patients with diabetes. Specifically, it found that CABG was more resource-intensive and expensive in patients with diabetes and that in-hospital adverse events and long-term survival were worse.
The same 2015 study also noted that Cleveland Clinic has seen the percentage of its CABG patients who have diabetes escalate from 7 percent in 1970 to more than 40 percent today.
Additionally, today’s CABG patient is older, on average, and more likely to have obesity, hypertension, peripheral arterial disease, chronic renal insufficiency, a poor lipid profile, a history of stroke and more advanced coronary artery disease. “We need to find a way to identify which factors most influence CABG outcomes in diabetic patients and then neutralize them in order to optimize CABG outcomes in this population,” Dr. Sabik notes.
Advertisement
In the current analysis, the superior patency for ITA grafts versus SV grafts at all time points in both diabetic and nondiabetic patients (see Table above) makes an excellent case in favor of internal thoracic artery grafting whenever possible, Dr. Sabik points out.
“The use of internal thoracic artery grafts should be maximized in all patients undergoing coronary surgery, because they have excellent patency in both diabetic and nondiabetic patients even 20 years after surgery,” he says.
Click here to view more clinical research presented at ACC.16.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable