A push for prolonged rhythm monitoring — and more thorough workup
If you mention cryptogenic stroke to a group of specialists, you might stir up disagreement on a point or two. But they’re apt to agree on at least one thing: This entity represents a diagnostic deficiency that stroke specialists hope to soon render far less common than it is today.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
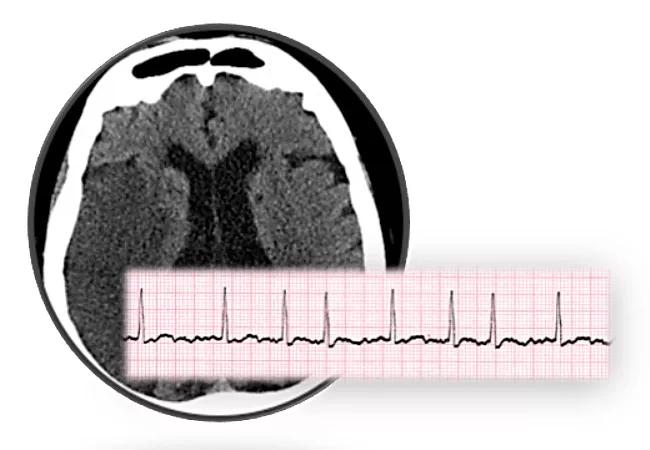
About one-third of all ischemic strokes — approximately 200,000 annually in the U.S. — are deemed “cryptogenic,” defined as a brain infarction for which a specific cause isn’t found despite extensive workup. Occult paroxysmal atrial fibrillation (AF) leading to cardiac embolism is thought to be a frequent cause, yet less than 3 percent of those cases are picked up on routine admission ECG, and a mere 3 to 7 percent more are detected on inpatient continuous telemetry and postdischarge 24-hour Holter monitoring.
Newer modalities — including 30-day mobile continuous outpatient telemetry (MCOT) and implantable loop recorders — have the potential to improve the yield considerably, but debate surrounds the optimal use of both of these technologies.
The stakes are high because patients who have AF are better treated with anticoagulants, which reduce the risk of a second stroke by 70 to 80 percent, than with antiplatelet medications, which lower the risk by only about 20 to 40 percent.
Since the arrival of newer anticoagulants that carry a lower bleeding risk than warfarin, some in the field argue that these agents should simply be given prophylactically in patients with cryptogenic stroke in whom AF is suspected. Studies are now being conducted to explore that practice, but it still carries risk.
“Why not just assume patients have atrial fibrillation and give them anticoagulants? Because it comes with a price — bleeding,” explains Walid Saliba, MD, Director of the Atrial Fibrillation Center and Associate Director of Cardiac Pacing and Electrophysiology at Cleveland Clinic. “The newer agents are safer, but they can still cause intracerebral or gastrointestinal bleeds. It’s potentially better to find atrial fib first and then put the patient on anticoagulation.”
Advertisement
From her vantage point as a stroke specialist in Cleveland Clinic’s Cerebrovascular Center, neurologist Irene Katzan, MD, often sees patients who have been diagnosed with cryptogenic stroke but haven’t had complete workups.
Standard testing for stroke includes the following:
“The proportion of patients who end up with the diagnosis of cryptogenic stroke is dependent on the extent of the evaluation done to determine the cause,” Dr. Katzan says. “There are many cases where not much is done to evaluate the cause of stroke.”
Sometimes the basics are done but there are no further evaluations when initial testing is negative. “Some tests are considered standard of care, but there are several additional tests if those are negative,” Dr. Katzan notes. “These are very individualized to the situation, and that’s where assessment can fall apart.”
Two recent randomized trials published in the New England Journal of Medicine point to the potential role for extended cardiac monitoring to identify AF in people with cryptogenic stroke or transient ischemic attack in whom AF wasn’t found on 24-hour ECG monitoring:
Advertisement
Dr. Saliba calls it “reasonable” to start with an MCOT device and, if that proves nonrevealing, to consider moving to the implantable. In fact, some insurers require that type of stepped approach. “The bottom line,” he adds, “is that the more you look, the more atrial fibrillation you’ll find.”
“There’s a push to go further and use prolonged rhythm monitoring,” Dr. Katzan adds. “That’s important, but we need to also step back and do as much as we can in the initial evaluation because even that could be improved.”
Debate has developed around which AF characteristics should be considered relevant to future stroke risk. But Dr. Saliba notes that for a patient who has already had a stroke, any degree of AF, no matter how brief or how long after the stroke, is enough to warrant anticoagulation. “In that situation, I wouldn’t worry how long they had it,” he says.
He’s quick to add that because of the bleeding risk, the patient must be informed about both benefits and risks: “All anticoagulation needs to involve shared decision-making.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable