Observational study supports adding CAC score to traditional risk factors for precision medicine approach
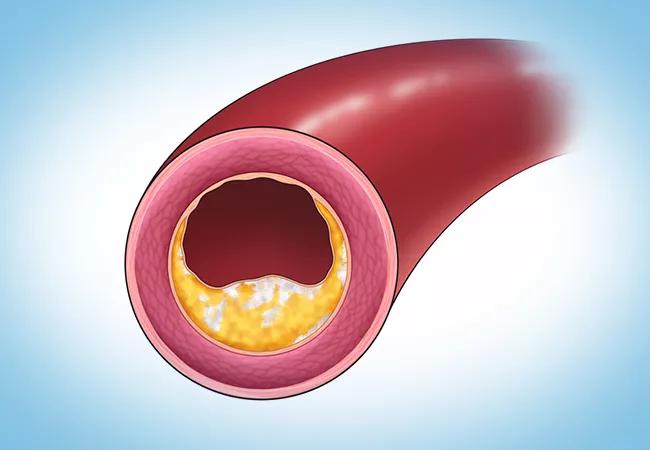
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bb0a672a-f1be-448a-af64-4d0d90d2750f/23-HVI-4194575_coronary-artery-calcium_650x450_jpg)
illustration of coronary artery with calcified plaque
Adding coronary artery calcium scoring to traditional screening for cardiovascular disease (CVD) increases the precision of 10-year risk calculations in individual patients. So suggests a new study by Cleveland Clinic researchers published in the American Journal of Cardiology (2023;206:303-308).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
According to the analysis of data from over 5,000 asymptomatic middle-aged adults, adding coronary artery calcium scoring (CACS) from the Multi-Ethnic Study of Atherosclerosis (MESA) to two traditional CVD risk scores — the Atherosclerotic Cardiovascular Disease Risk Calculator (ASCVD) and the Reynolds Risk Score (RRS) — resulted in significant stratification in nearly half of study participants. Overall, the ASCVD overestimated CVD risk while the RRS underestimated CVD risk compared with MESA-CACS. However, a differential reclassification emerged when participants were divided by number of calcified coronary arteries.
“Clearly, none of the currently available risk calculators stratifies individual risk perfectly, leading to the potential for misclassification of patients and under- or overprescribing of preventive therapy,” says the study’s senior and corresponding author, Milind Desai, MD, MBA, Vice Chair of Education for Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “But adding coronary artery calcium results to the traditional CVD risk models provides important and synergistic value, and can translate into precision medicine tailored to an individual patient’s best interests.”
The observational cross-sectional study included 5,324 consecutive individuals who underwent CACS as part of primary preventive screening of asymptomatic individuals in an executive health program at Cleveland Clinic between March 2016 and October 2021. Three-quarters of participants (75.6%) were male and 87.4% were white, with a median age of 57 years.
Advertisement
The investigators used information from participants’ medical history and laboratory workups to calculate their individual 10-year risk based on the ASCVD, the RRS and MESA-CACS.
Current guidelines for CVD risk classification and statin therapy initiation in middle-aged individuals focus on the ASCVD categorization. It relies solely on traditional Framingham Heart Study risk factors, such as age, gender, race and history of smoking, diabetes and hyperlipidemia. The RSS takes into consideration those factors plus family history of early CVD and systemic inflammation, while MESA-CACS also includes deposition of calcium in the individual’s coronary arteries.
The researchers next broke down the scores from the risk models into four categories of 10-year CVD risk:
Each study participant’s coronary arterial age also was calculated and compared with their chronological age.
Compared with the ASCVD, using MESA-CACS resulted in downgrading of CVD risk in 31% of participants and upgrading of risk in 14% of participants. Results were similar for comparison of MESA-CACS with the RRS: downgrading of CVD risk in 26% of subjects and upgrading of risk in 15% of subjects.
Notably, after stratifying participants by the number of coronary arteries affected by calcification, the authors found that the ASCVD overestimated CVD risk only in those with CAC in one or no coronary arteries and that MESA-CACS overestimated risk when CAC was present in two or more arteries. The RRS overestimated risk only in patients with no CAC while it underestimated risk in patients with any CAC.
Advertisement
“Dividing the patients based on number of calcified coronary arteries resulted in a differential and significant reclassification,” Dr. Desai notes, “and we found only a modest correlation between 10-year CVD risk by MESA-CACS versus the ASCVD and RRS.”
The researchers also assessed for any potential association between CACS and lipoprotein A (Lp[a]) and apolipoprotein B (ApoB), both of which are well-established predictors of increased CVD risk. Lp(a) distribution did not differ significantly among the MESA-CACS risk groups, whereas a modest correlation was found between ApoB and MESA-CACS risk scores.
“Higher levels of Lp(a) do not correlate with higher MESA-CACS 10-year risk score,” observes study co-author Leslie Cho, MD, Co-Section Head of Preventive Cardiology and Rehabilitation at Cleveland Clinic. “For this reason, measuring Lpa also could add independent and synergistic value to CVD risk stratification. We hypothesize that it may be useful for long-term cardiovascular prognostication in young adults.”
The authors believe that the collective study results may hold significant clinical implications. CACS is reliable, cost-effective and performed noninvasively with noncontrast cardiac CT. They caution, however, that while their sample size was large and the CAC measurement was standardized, the findings are limited by the observational nature of their study and its predominantly white and male population.
“More studies are needed to confirm the effectiveness of calcium quantification and Lp(a) measurement for assessment of CVD risk, but almost one-quarter of our population was already taking a statin despite having a CAC score of 0, which would have ruled out that therapy,” Dr. Desai notes. “Use of MESA-CACS in risk modeling might have spared these patients from long-term daily medication and the costs and potential side effects associated with it.”
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable