Radiation reduction measures, customized devices evolve

By Lourdes R. Prieto, MD, and Alex Golden, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Percutaneous interventions are playing an ever-increasing role in the care of patients with congenital heart disease. Many lesions previously requiring open heart surgery can now be treated less invasively on an outpatient basis with minimal recovery times.
This progress, while enthusiastically welcomed, gives rise to new challenges, including the need to limit radiation exposure from these interventions and to develop devices tailored to the small bodies of our youngest patients. Here we profile a few examples of how we are meeting these challenges in Cleveland Clinic Children’s Center for Pediatric and Congenital Heart Disease.
As procedures become more complex and patients require multiple catheterizations over a lifetime, radiation exposure becomes an important consideration. The Center for Pediatric and Congenital Heart Disease is committed to the principle of ALARA, or “as low as reasonably achievable,” when delivering radiation in the catheterization laboratory.
We have worked with Siemens Healthcare to update one of our two catheterization laboratories with the newest available detector technology, the Artis Q.zen angiography system, approved by the FDA in March 2013. This system, which includes a crystalline silicon detector, reduces electronic noise, allowing imaging at much lower radiation levels than previously possible.
In addition to reducing radiation exposure to ultralow levels, the system is equipped with Siemens’ newly developed GIGALIX X-ray tube, which uses flat emitter technology to provide small focal sizes and strong, short X-ray pulses. The result is improved contrast and spatial resolution of small moving vessels. The laboratory is projected to be completed by the end of 2013.
Advertisement
Another crucial factor in lowering radiation exposure is reducing procedure times. To that end, we are testing pediatric applications of a 3-D/2-D registration technology (syngo iGuide Toolbox, Siemens Healthcare) that allows anatomic structures from a prior cardiac MRI or CT to be superimposed onto fluoroscopic images. This technology facilitates access to a desired structure — for example, a collateral vessel, pulmonary artery branch or pulmonary vein — by providing a road map visible on fluoroscopy. It will likely result in decreased radiation exposure and reduced contrast administration.
In the catheterization lab we have the capability to perform rotational angiography (Figure 1), which reveals the 3-D anatomy of a structure, improving the diagnostic quality of the procedure and enabling more accurate selection of the best angiographic angles for a given intervention. This 3-D data set also makes it possible to register the location of a vessel on fluoroscopy, reducing the time and radiation needed to access a desired structure.
Along with implementing the latest technology to minimize radiation while optimizing image quality, our interventional group is participating in the testing and development of leading edge technologies to continue to advance pediatric cardiac intervention.
We are now enrolling patients in the GORE® Septal Occluder (GSO) Clinical Study to evaluate the safety and efficacy of a newly designed atrial septal defect closure device with many advantages over its predecessor, the HELEX® Septal Occluder (W.L. Gore & Associates). The GSO delivery mechanism significantly improves ease of use. Other design features enhance device apposition to the atrial septum and tissue response, which will likely increase atrial septal defect closure rates while also improving safety.
Advertisement
Cardiac catheterization in infants is limited by the size of the sheath that can be safely inserted in the femoral artery for vascular access. Use of larger sheaths can result in significant complications, including arterial occlusion with compromised perfusion to the leg.
Our pediatric interventional cardiology group has worked with a nonprofit company, PediaWorks/PediaVascular, to design a system of 3-French intravascular catheters (Figure 2). 3-French catheters were previously available but did not allow accurate pressure measurements or adequate angiograms and were therefore rarely used. The FDA cleared the new catheters in January 2013, making these the only intravascular catheters approved specifically for pediatric use in the U.S. These catheters enable us to obtain hemodynamic information and perform angiography more safely than ever before. Cleveland Clinic Children’s was the first hospital in the world to use these new catheters.
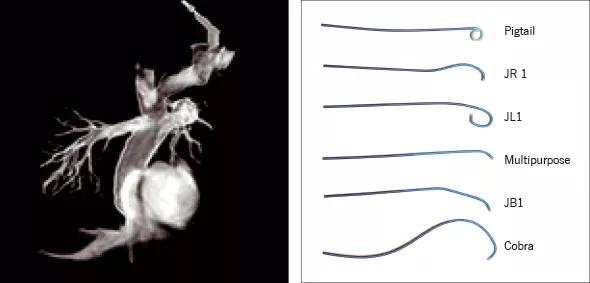
Figure 1. Three-dimensional rotational angiography following a fenestrated extracardiac Fontan procedure in a 5-year-old girl with hypoplastic left heart syndrome. The fenestration was subsequently closed with a device. This type of 3-D imaging can be used as a real-time map for live guidance during procedures.
Figure 2. The Mongoose® 3-French catheters developed by PediaWorks/PediaVascular with assistance from Cleveland Clinic Children’s pediatric cardiologists. These are the first intravascular catheters cleared by the FDA specifically for use in children.
Advertisement
Since we began our percutaneous pulmonary valve program in 2010, we have placed these valves (Figure 3) in 37 patients ranging in age from 8 to 61 years. The Melody® Transcatheter Pulmonary Valve (Medtronic), the only FDA-approved percutaneous pulmonary valve, has been successfully implanted in all these patients, with no significant complications. Follow-up, now exceeding three years for the earliest patients, continues to demonstrate excellent valve function, with no patient requiring repeat intervention.

Figure 3. Angiograms before (top) and after (bottom) placement of a Melody Transcatheter Pulmonary Valve in a 16-year-old with narrowing of a conduit from the right ventricle to the pulmonary artery. After placement of the valve, the narrowing was eliminated.
As a crucial safeguard in performing these procedures, we participate in a multi-institutional study that allows us access to covered stents in the rare case of a disruption in the conduit from the right ventricle to the pulmonary artery during preparation to implant the valve. These stents, which are not currently FDA-approved, are available to only a select group of institutions.
Dr. Prieto is Director of Pediatric Catheterization Laboratory in the Center for Pediatric and Congenital Heart Disease. Her specialty interests include interventional catheterization in patients with congenital heart disease and pulmonary vein stenosis.
Dr. Golden is a pediatric cardiologist in the Center for Pediatric and Congenital Heart Disease. His specialty interests include diagnostic and interventional cardiac catheterization and congenital heart disease.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable