Experts weigh in on proposed changes to reimbursement requirements

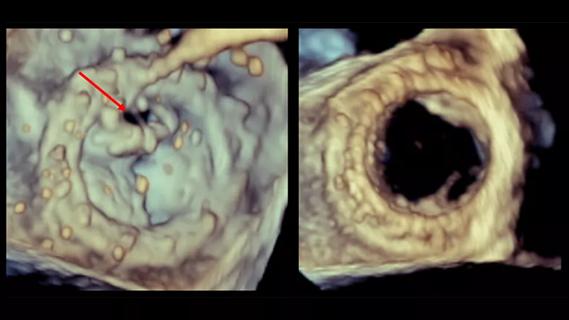
The Centers for Medicare & Medicaid Services (CMS) should add quality outcome measures to determine qualification for coverage for institutions and heart teams performing transcatheter aortic valve replacement (TAVR) procedures. So argue leaders of Cleveland Clinic’s TAVR team in anticipation of the CMS decision on changes to the National Coverage Determination (NCD), which were set in 2012, with the next NCD expected by June 25, 2019.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A panel of the Medicare Evidence Development & Coverage Advisory Committee (MEDCAC), which reviewed evidence and opinions July 25, 2018, following a public comment period (see comments here), did not reach consensus on a variety of issues, particularly regarding procedural volume requirements for qualification for CMS coverage.
“The quality of patient care should be the paramount consideration for TAVR coverage,” urges cardiothoracic surgeon Lars Svensson, MD, PhD, Chairman of Cleveland Clinic’s Miller Family Heart & Vascular Institute. “Coverage must be based on measures of how well a team or hospital performs and not just the number of procedures they handle annually.”
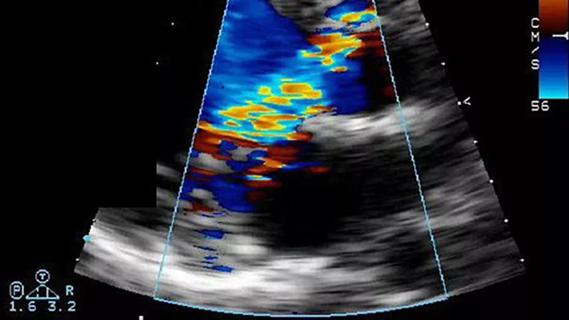
Samir Kapadia, MD, Cleveland Clinic’s Section Head of Invasive and Interventional Cardiology, concurs, noting that quality standards for maintaining certification should be set at annual rates of no more than 4 percent for mortality and 2 percent for strokes for all patients undergoing isolated elective aortic valve replacement, whether TAVR or surgical aortic valve replacement (SAVR). “This type of combined responsibility for outcomes of SAVR and TAVR for a center will build stronger heart teams, and patients will get best possible treatments,” he says.
“Heart teams and institutions are required to routinely submit their outcomes data to the Transcatheter Valve Therapies [TVT] Registry to prove they meet these standards,” adds Dr. Kapadia. “Data should be more transparent and made available to CMS and insurers, and possibly to other interested parties.”
Advertisement
The Society for Thoracic Surgeons (STS) and American College of Cardiology (ACC) currently monitor patient safety and outcomes related to transcatheter valve replacement and repair procedures through their TVT Registry, including all-cause mortality, strokes, TIAs, acute kidney injury, repeat aortic valve procedures and quality-of-life measures. The registry is used by CMS to determine requirements for TAVR coverage decisions, but decisions are currently based only on quantity of procedures.
MEDCAC is considering eliminating existing volume requirements to increase access. Several physicians from small hospitals in remote areas argued in their public comments that the current volume requirements for TAVR prevent their patients from receiving this lifesaving procedure.
However, Dr. Kapadia counters that the procedure is usually done electively, not emergently, and involves only a short hospital stay, so concentrating care at major centers should be a practical option. Currently the U.S. has more than 550 active TAVR sites.
“We support maintaining volume requirements for coverage, although they could probably be safely reduced to some extent,” he asserts. “Patients are best served by getting TAVR done at a center with adequate experience and then returning to their local physician for follow-up care.”
Under existing coverage requirements, CMS recognizes the importance of patients being under the care of a heart team. Drs. Svensson and Kapadia strongly support the team-care concept but argue that some details should be changed.
Advertisement
Currently, CMS requires that two cardiac surgeons evaluate each patient independently to document suitability for TAVR. Drs. Svensson and Kapadia believe the opinion of one surgeon should suffice.
“An institution’s heart team should be responsible for properly allocating patients to TAVR and SAVR,” says Dr. Svensson. “Patient assessment by one cardiac surgeon and one interventional cardiologist should be adequate. Requiring two cardiac surgeons to be involved in the decision is unnecessary.”
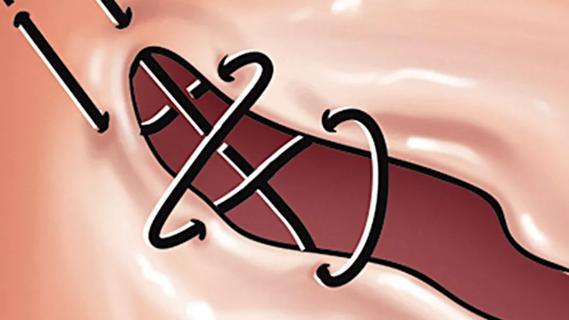
Current CMS policy also states that the heart team’s interventional cardiologist and cardiac surgeon “must jointly participate in the intraoperative technical aspects of TAVR.” Drs. Svensson and Kapadia would strengthen this requirement.
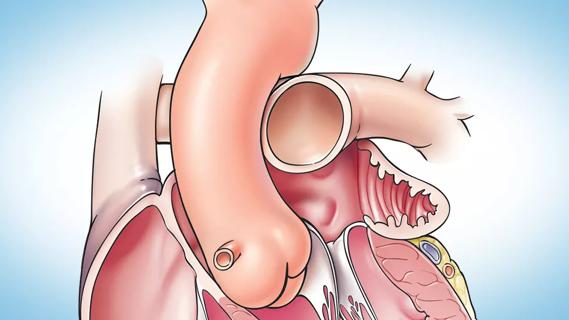
“A cardiac surgeon should be scrubbed and in the operating room during all TAVR procedures,” says Dr. Kapadia. “This is essential to provide expeditious surgical solutions for potential serious complications such as annular rupture or aortic dissection. Further, participation in the procedure completes the loop from assessment to treatment, which is critical for well-being of the heart team. ”
Reimbursement rates are not on the table in the current MEDCAC considerations, but Dr. Svensson argues that the issue needs addressing. He notes that discrepancies in current reimbursement rates according to geographic region make it prohibitive for some hospitals to undertake TAVR programs, especially those in the middle of the country.
“CMS coverage may not even cover the total cost of the device, the filter and, when needed, a pacemaker,” Dr. Svensson says. “Current differential reimbursement rates are unfairly limiting access.”
Advertisement
To inform the MEDCAC panel, several leading U.S. cardiac surgery and cardiology societies recently developed a consensus document on operator and institutional recommendations and requirements for TAVR. The document was co-published in several specialty journals (see it here).
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
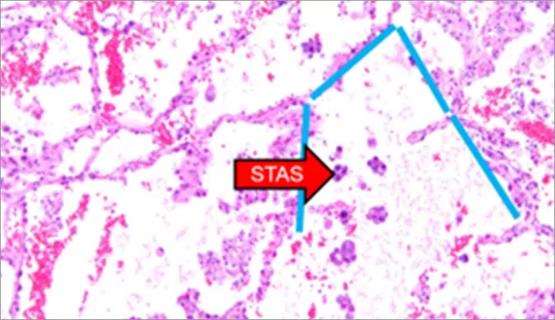
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable