Meticulous surgical methods produce good outcomes

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A history of previous surgery formerly was considered one of the relative contraindications for laparoscopic surgery because of higher risk for port trocar injuries, perioperative complications and prolonged operative time due to adhesiolysis.
With increased laparoscopic experience, refinement of surgical techniques and improved instrumentation, laparoscopic surgery has been extended to patients with previous abdominal surgery. Here, we focus on our single-center experience with robot-assisted laparoscopic partial nephrectomy (RALPN) in patients with a history of previous abdominal surgery.
The study population was retrieved from our ongoing Institutional Review Board-approved, prospectively maintained database. The medical records of patients who underwent RALPN from June 2006 to February 2013 were reviewed. Patients were divided into two groups: those who had history of previous abdominal surgery and those with no previous abdominal surgery. The two study groups were compared in terms of baseline patient characteristics and tumor characteristics, as well as in terms of operative outcomes and intraoperative and postoperative complications.
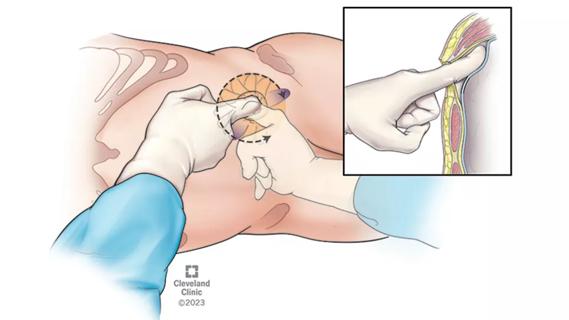
In the setting of previous abdominal surgery, few modifications to our standard RALPN technique are adopted. We place the access point of the Veress needle as far as possible from the incision site, usually 4 cm to 5 cm away from a previous surgery incision site. An alternative access point is 4 cm to 5 cm cranial and medial to the anterior superior iliac spine if it is a scar-free area.
Advertisement
We perform a positive drop test and confirm low initial insufflation pressure before proceeding with pneumoperitoneum. In case of doubt, we employ an open Hassan technique for placement of ports. The abdominal cavity is insufflated to 15 mm Hg. We introduce a 12 mm camera port and examine the cavity for visceral injuries or adhesions.
Adhesions are taken down sharply using laparoscopic scissors if encountered in the site of placement of other ports. If the adhesions are located medially, we place lateral ports and adhesions can be taken down sharply. A 3- or 4-port configuration can be used, depending on the surgeon’s preference.
We complete the rest of the procedure by following the standard steps, including bowel mobilization, identification of the ureter and gonadal vessels, exposure of the psoas muscle, identification and dissection of the hilum, defatting of the kidney, tumor identification, intraoperative ultrasound, scoring of tumor margins, hilar clamping (when necessary), tumor excision, and renorrhaphy.
Of 587 patients who underwent RALPN during the study period, five were excluded due to incomplete documentation. Overall, 348 patients (59.2 percent of total) had a history of previous abdominal surgery (Table 1). The two study groups were comparable in terms of age, body mass index, American Society of Anesthesiologists (ASA) score, Charlson comorbidity index, tumor size and laterality. Renal nephrometry score was higher in patients with previous surgery compared with those with negative surgical history (7.3 vs. 7, p = 0.04).
Advertisement
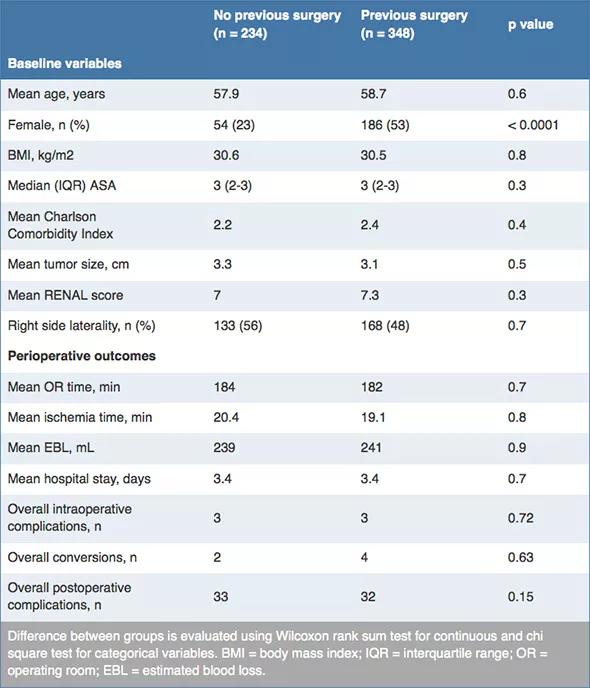
Table 1. . RALPN in patients with previous abdominal surgery: comparative outcomes
There was no difference in operative time, warm ischemia time or estimated blood loss. Surgical access was accomplished using a Veress needle in all but three patients. There were no complications related to gaining pneumoperitoneum, placement of robotic ports or takedown of peritoneal adhesions.
In conclusion, although performing RALPN in the setting of previous abdominal surgery can be challenging, with sound surgical techniques in gaining access, placing ports and performing meticulous adhesiolysis, the procedure can be safely completed and can provide surgical outcomes comparable to those of patients with negative surgical history.
Dr. Kaouk is Director of Cleveland Clinic Glickman Urological & Kidney Institute’s Center for Robotic and Laparoscopic Surgery and is the Urological & Kidney Institute’s Vice Chair for Surgical Innovations. He is a Professor of Surgery at Cleveland Clinic Lerner College of Medicine.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients