Providers must inform patients of guarded prognosis
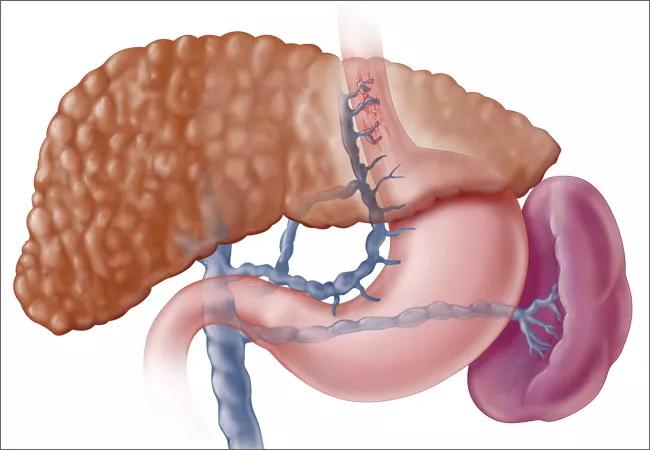
Patients with cirrhosis often develop varicose veins of the esophagus and stomach due to high pressure in the liver that causes portal vein hypertension. If the varices rupture, these patients often need endoscopic intervention to stop the bleeding such as endoscopic variceal banding.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In severe cases, however, such interventions might not work and patients may need transjugular intrahepatic portosystemic shunt (TIPS), a procedure that uses imaging guidance to place a stent that connects the portal vein to the hepatic vein in the liver. This diverts blood away from the liver and relieves the pressure.
TIPS, however, has its own risks. “Unfortunately when liver function is compromised there’s a risk of acute on chronic liver failure (ACLF) with risk of mortality, as the liver might not tolerate the low perfusion of blood after TIPS placement” said Jamak Modaresi Esfeh, MD, gastroenterology and transplant hepatology, Cleveland Clinic.
Dr. Esfeh and colleagues recently conducted a retrospective study of patients who underwent TIPS for refractory variceal bleed between 2013 and 2017 at the Cleveland Clinic to determine whether the patients’ score on the Model of End-Stage Liver Disease (MELD-Na) predicted outcome after TIPS. They presented their results today at the 2018 American College of Gastroenterology meeting in Philadelphia.
The investigators looked at 75 patients with variceal bleeding who despite endoscopic intervention with a mean of 2 scopes prior to TIPS. Thirty of the patients had a high MELD-Na score and 45 had a low MELD-Na score.
The patients average age was 55±13 and 64 percent were male. The 40 percent of patients with a high MELD-Na score, had scores ranging between 15 and 48 with a mean of 24±7.8. The 60 percent with a low MELD-Na score had scores ranging between 6 and 14 with a mean of 9.4± 2.
Advertisement
In the high MELD-Na group, 11 patents were Child-Turcotte-Pugh (CTP) Class B and 19 were C. In the low MELD-Na group, 13 were CTP A, 31 CTP B and 1 CTP C.
The most common complications after TIPS for the high MELD-Na group versus the low MELD-Na group included acute kidney injury (37 percent versus 0 percent), infection (23 percent versus percent), hepatic encephalopathy (23 percent versus. 4 percent), and hemorrhagic shock (27 percent versus 2 percent).
Patients in the high MELD-Na group required an average of four units of blood in the first 48 hours while those with a low score required two. Those in the high MELD-Na group also had longer post-TIPS intubation time (3 days versus 1 day) and a longer ICU stay (4 days versus 3 days).
Post-TIPS follow up ranged from 0 to 55.6 months with a median of 7.8 months. A total of 16 patients (12 during TIPS hospitalization) in the high MELD-Na group and 9 (2 during TIPS hospitalization) in the low MELD-Na group died.
The results indicate that patients with a MELD-Na score of 15 or higher do worse after TIPS placement for endoscopic refractory variceal bleed and that the MELD-Na score is a reliable predictor for risk stratification and survival after emergent TIPS.
“It’s a complicated situation,” said Dr. Esfeh. “We need to communicate the risks carefully to the patient and family and let them know that TIPS can help with the bleeding but there is also risk of mortality.”
Advertisement
Advertisement

Strong patient communication can help clinicians choose the best treatment option

ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance

The importance of raising awareness and taking steps to mitigate these occurrences

New research indicates feasibility and helps identify which patients could benefit

Treating a patient after a complicated hernia repair led to surgical complications and chronic pain

Standardized and collaborative care improves liver transplantations

Fewer incisions and more control for surgeons

Caregiver collaboration and patient education remain critical