Differences between large-medium vessel and small vessel variants
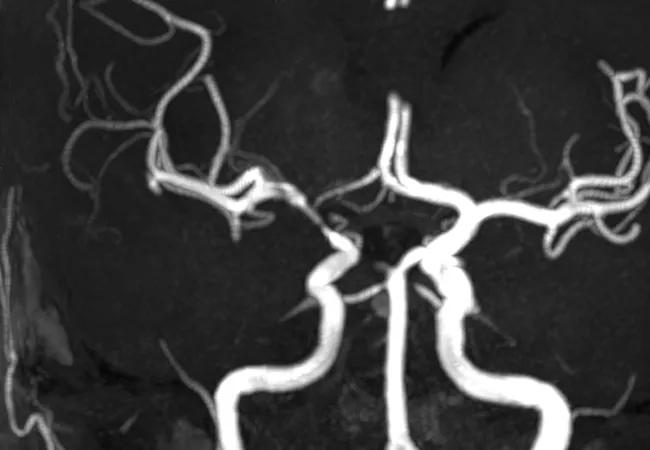
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c66b8908-9c2e-49fa-a1a4-62d9c2214c04/17-RHE-1241-Hajj-Ali-Hero-Image-650x450pxl_jpg)
Imaging of vessels in CNS vasculitis
By Ken Uchino, MD, Leonard Calabrese, DO, and Rula Hajj-Ali, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Arriving at a diagnosis of central nervous system vasculitis (CNS-V) is fraught with challenges. Clinical presentation can be quite variable, and there is no classic presentation. Further complicating matters, the condition has several mimics, brain tissue is inaccessible and there is no disease-specific test. However, advances in neuroimaging and next-generation sequencing — along with the involvement of a multidisciplinary clinical team — have added formidably to our knowledge of CNS-V.
Recently, two different disease subtypes have been postulated: the small vessel variant (SVV) and large-medium vessel variant (LMVV).1 We sought to clarify the clinical characteristics, brain MRI findings and diagnostic accuracy of high-resolution vessel wall image (HR-VWI) and brain biopsy according to the affected vessel size in CNS-V patients. We discuss the results of this study in a poster presented at ACR Convergence 2020.2
Using Cleveland Clinic’s CNS vasculopathy registry, we identified 34 CNS-V patients who underwent digital subtraction angiography (DSA) or magnetic resonance angiography (MRA) at our institution from 2012-2019. For this study, patients with cerebral vasculature indicating vasculitis in proximal or middle arterial segments had LMVV, and patients with only smaller distal branch vessel involvements or normal angiography had SVV.
Based on angiographical findings, 11 (32.4%) of the patients in our cohort were LMVV and 23 (67.6%) were SVV. Patients with LMVV had more infarcts and were more likely to have concentric vessel wall enhancement (VWE) on HR-VWI, as shown in Table 1. Meningeal/parenchymal contrast enhancement of lesion was more frequently observed in the SVV group, and the majority of patients in this group were diagnosed by brain biopsy, as shown in Table 2. Brian biopsy was positive in 100% of patients with SVV compared with only 57.1% in patients with LMVV.
Advertisement
| LMVV(n = 11) | SVV(N = 23) | P Value | |
|---|---|---|---|
| MRI findings, n (%) | |||
| Brain infarcts | 11 (100.0) | 14 (60.9) | 0.017 |
| Parenchymal hemorrhage | 1 (9.1) | 5 (21.7) | 0.638 |
| Subarachnoid hemorrhage | 0 (0.0) | 4 (17.4) | 0.280 |
| White matter lesion | 2 (18.2) | 12 (52.2) | 0.076 |
| Tumor-like lesion | 0 (0.0) | 8 (34.8) | 0.034 |
| Contract enhancement lesion | 5 (45.5) | 20 (87.0) | 0.033 |
| Assessment of the cerebral vascular image, n (%) | |||
| Both MRA and DSA | 11 (100.0) | 13 (56.5) | 0.014 |
| Only MRA | 0 (0.0) | 8 (34.8) | 0.034 |
| Only DSA | 0 (0.0) | 2 (8.7) | 1.000 |
| Arterial stenosis, n (%) | |||
| Proximal segment | 7 (63.6) | 0 (0.0) | < 0.001 |
| Middle segment | 10 (90.9) | 0 (0.0) | < 0.001 |
| Smaller distal branch | 10 (90.0) | 8 (34.8) | 0.003 |
| None | 0 (0.0) | 15 (62.5) | < 0.001 |
| HR-VWI findings, n (%) | |||
| VWE | 10 (100.0) [n = 10] | 2 (14.2) [n = 14] | < 0.001 |
| Concentric VWE | 9 (90.0) [n = 10] | 1 (7.1) [n = 14] | < 0.001 |
| Eccentric VWE | 1 (10.0)[n = 10] | 1 (7.1) [n = 14] | 1.000 |
| LMVV(n = 11) | |||
| MRI findings, n (%) | |||
| Brain infarcts | |||
| SVV(N = 23) | |||
| 11 (100.0) | |||
| P Value | |||
| 14 (60.9) | |||
| 0.017 | |||
| Parenchymal hemorrhage | |||
| SVV(N = 23) | |||
| 1 (9.1) | |||
| P Value | |||
| 5 (21.7) | |||
| 0.638 | |||
| Subarachnoid hemorrhage | |||
| SVV(N = 23) | |||
| 0 (0.0) | |||
| P Value | |||
| 4 (17.4) | |||
| 0.280 | |||
| White matter lesion | |||
| SVV(N = 23) | |||
| 2 (18.2) | |||
| P Value | |||
| 12 (52.2) | |||
| 0.076 | |||
| Tumor-like lesion | |||
| SVV(N = 23) | |||
| 0 (0.0) | |||
| P Value | |||
| 8 (34.8) | |||
| 0.034 | |||
| Contract enhancement lesion | |||
| SVV(N = 23) | |||
| 5 (45.5) | |||
| P Value | |||
| 20 (87.0) | |||
| 0.033 | |||
| Assessment of the cerebral vascular image, n (%) | |||
| Both MRA and DSA | |||
| SVV(N = 23) | |||
| 11 (100.0) | |||
| P Value | |||
| 13 (56.5) | |||
| 0.014 | |||
| Only MRA | |||
| SVV(N = 23) | |||
| 0 (0.0) | |||
| P Value | |||
| 8 (34.8) | |||
| 0.034 | |||
| Only DSA | |||
| SVV(N = 23) | |||
| 0 (0.0) | |||
| P Value | |||
| 2 (8.7) | |||
| 1.000 | |||
| Arterial stenosis, n (%) | |||
| Proximal segment | |||
| SVV(N = 23) | |||
| 7 (63.6) | |||
| P Value | |||
| 0 (0.0) | |||
| < 0.001 | |||
| Middle segment | |||
| SVV(N = 23) | |||
| 10 (90.9) | |||
| P Value | |||
| 0 (0.0) | |||
| < 0.001 | |||
| Smaller distal branch | |||
| SVV(N = 23) | |||
| 10 (90.0) | |||
| P Value | |||
| 8 (34.8) | |||
| 0.003 | |||
| None | |||
| SVV(N = 23) | |||
| 0 (0.0) | |||
| P Value | |||
| 15 (62.5) | |||
| < 0.001 | |||
| HR-VWI findings, n (%) | |||
| VWE | |||
| SVV(N = 23) | |||
| 10 (100.0) [n = 10] | |||
| P Value | |||
| 2 (14.2) [n = 14] | |||
| < 0.001 | |||
| Concentric VWE | |||
| SVV(N = 23) | |||
| 9 (90.0) [n = 10] | |||
| P Value | |||
| 1 (7.1) [n = 14] | |||
| < 0.001 | |||
| Eccentric VWE | |||
| SVV(N = 23) | |||
| 1 (10.0)[n = 10] | |||
| P Value | |||
| 1 (7.1) [n = 14] | |||
| 1.000 |
Notes: LMVV = large-medium vessel variant; SVV = small vessel variant; MRA = magnetic resonance angiography; DSA = digital subtraction angiography; HR-VWI = high-resolution vessel wall image; VWE = vessel wall enhancement
| LMVV(n = 11) | SVV( n = 23) | P Value | |
|---|---|---|---|
| Biopsy proven CNS-V, n (%) | 4 (36.4) | 18 (78.3) | 0.026 |
| Biopsy positive, n (%) | 4 (57.1) [n = 7] | 18 (100.0) [n = 18] | 0.015 |
| Pathological patterns, n (%) | |||
| Granulomatous vasculitis | 1 (14.3) [n = 7] | 1 (11.1) [n = 18] | 0.490 |
| Lymphocytic vasculitis | 3 (42.9) [n = 7] | 12 (66.7) [n = 18] | 0.378 |
| Necrotizing vasculitis | 0 (0.0) [n = 7] | 5 (27.8) [n = 18] | 0.274 |
| CSF findings, n (%) | |||
| Abnormal* | 11 (100.0) [n = 11] | 16 (80.0) [n = 20] | 0.269 |
| Pleocytosis* | 10 (90.9) [ n = 11] | 12 (60.0) [n = 20] | 0.106 |
| Elevated protein* | 8 (72.7) [n = 11] | 13 (65.0) [n = 20] | 1.000 |
| LMVV(n = 11) | |||
| Biopsy proven CNS-V, n (%) | |||
| SVV( n = 23) | |||
| 4 (36.4) | |||
| P Value | |||
| 18 (78.3) | |||
| 0.026 | |||
| Biopsy positive, n (%) | |||
| SVV( n = 23) | |||
| 4 (57.1) [n = 7] | |||
| P Value | |||
| 18 (100.0) [n = 18] | |||
| 0.015 | |||
| Pathological patterns, n (%) | |||
| Granulomatous vasculitis | |||
| SVV( n = 23) | |||
| 1 (14.3) [n = 7] | |||
| P Value | |||
| 1 (11.1) [n = 18] | |||
| 0.490 | |||
| Lymphocytic vasculitis | |||
| SVV( n = 23) | |||
| 3 (42.9) [n = 7] | |||
| P Value | |||
| 12 (66.7) [n = 18] | |||
| 0.378 | |||
| Necrotizing vasculitis | |||
| SVV( n = 23) | |||
| 0 (0.0) [n = 7] | |||
| P Value | |||
| 5 (27.8) [n = 18] | |||
| 0.274 | |||
| CSF findings, n (%) | |||
| Abnormal* | |||
| SVV( n = 23) | |||
| 11 (100.0) [n = 11] | |||
| P Value | |||
| 16 (80.0) [n = 20] | |||
| 0.269 | |||
| Pleocytosis* | |||
| SVV( n = 23) | |||
| 10 (90.9) [ n = 11] | |||
| P Value | |||
| 12 (60.0) [n = 20] | |||
| 0.106 | |||
| Elevated protein* | |||
| SVV( n = 23) | |||
| 8 (72.7) [n = 11] | |||
| P Value | |||
| 13 (65.0) [n = 20] | |||
| 1.000 |
Notes: CSF = cerebral spinal fluid; SNS-V = central nervous system vasculitis; LMVV = large/medium vessel variant; SVV = small vessel variant.
*Abnormal CSF is defined by either leukocyte counts > 5 cells/mm3 (pleocytosis) or protein level > 45 mg/dl (elevated protein).
Diagnostic approach for CNS-V depends on the affected vessel size. In LMVV patients, the diagnosis of CNS-V is mainly based on evidence of concentric VWE on HR-VWI. By contrast, brain biopsy should be considered in patients with suspected SVV CNS-V if parenchymal enhancement of lesion is detected. In patients without VWE on HR-VWI and targeting contrast enhancement lesion, careful assessments including CSF abnormalities, DSA findings and clinical pictures are needed for the diagnosis of the CNS-V.
We take a systematic approach to the work-up of any patient suspected to have CNS-V. This approach includes a general history and physical exam, with a thorough review of symptoms associated with systemic autoimmune disease. Clinicians should look for infectious and/or malignant conditions that might be associated with many of these nonspecific symptoms, especially fever, malaise, joint pains and weight loss. When CNS-V is suspected, brain biopsy is of high yield.
Advertisement
Advertisement
New study advances understanding of patient-defined goals
Testing options and therapies are expanding for this poorly understood sleep disorder
Real-world claims data and tissue culture studies set the stage for randomized clinical testing
Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH
Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond
Findings challenge dogma that microglia are exclusively destructive regardless of location in brain
Neurology is especially well positioned for opportunities to enhance clinical care and medical training
New review distills insights from studies over the past decade