A Glimpse into the Future of Spine Surgery
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Degenerative arthritis of the spine is a common ailment. It is a frequent cause of pain and missed work, with the most advanced cases presenting with neurological deficits. Nowhere is this condition more salient than in the cervical spine, where compression of the spinal cord can lead to paralysis. Available treatments are good at relieving symptoms, but none address the underlying problem of degenerative disk disease.
As with so many illnesses, treatments for degenerative spinal disease have improved incrementally over time. However, there has been no revolution in recent years that has fundamentally changed the way most doctors approach the disease. Such a treatment would not only provide relief of symptoms, but would also slow or even reverse the course of the degenerative process. Cervical artificial disk replacement, also known as arthroplasty, has shown promise over the past decade as an encouraging step in this direction.
The practice of medicine is best when it restores the body to its natural state.
At its core, degenerative spinal disease is a progressive loss of the structure and function of the intervertebral disk and other soft tissue components of the spine. The disks lose their height and elasticity, reducing the spine’s mobility and accelerating arthritic changes such as osteophyte formation.
The body cannot heal damaged spinal disks because they have no blood supply.
Severe degenerative disk problems can lead to frank disk herniation and osteophytosis. These structures can compress the spinal nerves and even the spinal cord, leading to pain and sometimes neurological deficits. When present, such deficits can progress and fail to respond to intervention. Continued loss of disk height may result in kyphosis, which further stresses the spine and accelerates the degenerative process.
Advertisement
Conservative treatments, including nonsteroidal medications, physical therapy and epidural steroid injections, all are effective at relieving symptoms. Unfortunately, they do little to stop the underlying deterioration.
A significant fraction of patients with cervical disk problems fail to improve with conservative, nonoperative treatment. For those patients who require surgery, the operation most commonly recommended is anterior cervical diskectomy and fusion. This technique involves removing the cervical disk and osteophytes and placement of a bone graft and metal plate to replace the disk, which ultimately results in biological fusion. Compression of neural elements is relieved, and the arthritic process is arrested between the operated vertebrae once fusion occurs. The success rate of this operation in terms of symptomatic pain relief is among the highest in spine surgery.
While fusion represents success, it is also the procedure’s primary drawback. Once vertebrae are fused, there is no mobility between them and neck stiffness increases. As these patients age, the symptoms of arthritis only worsen. Some will develop degenerative disks between other vertebrae that will then require additional surgery. If more fusions are performed, neck stiffness increases even more. And fusion is irreversible.
The elegance of successfully replacing a poorly functioning part with a better functioning one cannot be overstated. Cervical disk replacement or arthroplasty has been available in the United States for a decade as an accepted alternative to fusion and has been performed by Cleveland Clinic surgeons for nearly as long.
Advertisement
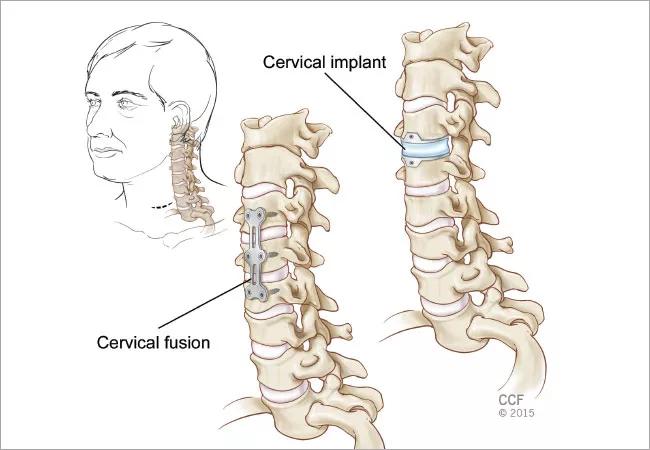
The approach to the spine is identical, including decompression of nerves and the spinal cord. As the illustration at right shows, the difference comes at the end of the surgery. Instead of placing a bone graft and immobilizing metal plate, the surgeon inserts the artificial disk into the space where the biological disk has been removed. The artificial disk is then secured to the native bone with screws. This concludes the procedure, the incision is closed and the patient is sent to recovery.
Patients typically spend one night in the hospital, similar to traditional fusion. Follow-up is provided in the weeks and months following surgery, with the patient completing physical therapy as needed and typically returning to normal activity within six weeks.
The artificial disk is mobile and preserves the patient’s ability to move his or her neck. In some cases, neck movement is actually improved. Over time, this creation of a more normal neck physiology may slow the degenerative process.
Available studies going back seven years show that cervical disk replacement improves neck pain, arm pain and neurological deficits at least as well as fusion.1
Cervical arthroplasty is a relatively new technology. It is likely to improve, and at a more rapid pace than the established technique of cervical fusion. New implants will improve on existing models, providing greater benefits to patients. In the future, disk replacements might be plastic, hybrid plastic/metal or even biological.
The move from fusion to disk replacement represents a potential paradigm shift. Arthritic hip joints were once fused, but are now replaced with functional joints that provide patients with an improved quality of life.
Advertisement
At present, cervical arthroplasty is performed far less frequently than fusion — but it is by no means a fad. Early adopters have pioneered arthroplasty and proved its success. In the future, it is likely we will view spine surgery as restorative instead of restrictive. Innovations such as facet joint replacement in conjunction with better disks will undoubtedly further slow spinal degeneration and bring an improved quality of life to those afflicted.
Paradigm shifts require the new model and process to provide a clear improvement over the standard. Cervical arthroplasty certainly satisfies this requirement.
Dr. Amps is a spine surgeon in the Center for Spine Health. He can be contacted at ampsj@ccf.org or 216.671.2205.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade