One of first reported successful uses of telaprevir in this setting
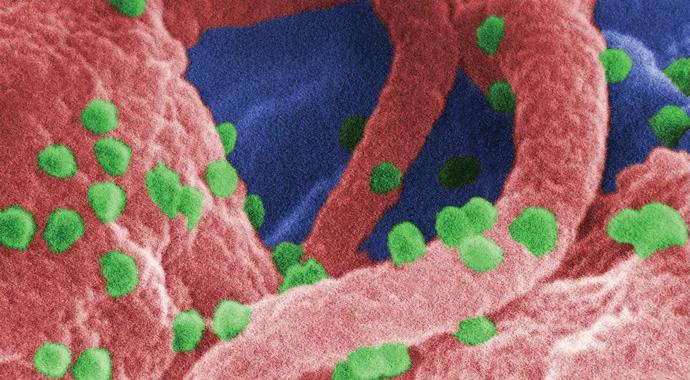
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/53b328e1-cc59-46aa-b889-f59faff9daa6/CDC_690x380_jpg)
CDC_690x380
By Bijan Eghtesad, MD, and Naim Alkhouri, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 62-year-old man with a history of HIV infection, chronic hepatitis C virus (HCV) genotype 1b infection complicated by cirrhosis, and hepatocellular carcinoma underwent liver transplantation at Cleveland Clinic. Nine months post-transplant, liver biopsy revealed recurrent hepatitis C infection with grade 2/4 inflammation and stage 2/4 fibrosis.
The patient’s immunosuppression regimen consisted of tacrolimus and mycophenolate mofetil. To address his HCV recurrence while accounting for these immunosuppressants, the team tried triple therapy with the direct-acting protease inhibitor telaprevir plus ribavirin and pegylated interferon.
To avoid having the patient on both HCV and HIV protease inhibitors, the darunavir-ritonavir component of his highly active antiretroviral therapy (HAART) regimen for HIV was stopped before telaprevir was started, at which time the integrase inhibitor raltegravir was also initiated.
From the onset of telaprevir-based therapy, the patient’s serum tacrolimus level was monitored very closely. Despite the need for frequent adjustments to his tacrolimus dosage, management was successful. At eight weeks, his HCV RNA became undetectable and remained undetectable 12 weeks after his 48-week HCV treatment regimen ended, indicating sustained virologic response. No harmful effects to the liver graft or to renal function were seen.
Two months after the end of telaprevir therapy, the patient was switched back to his original HAART regimen. More than one year later, his HIV and HCV levels remained undetectable.
Advertisement
This case was described in one of the first published reports of telaprevir use to treat HCV recurrence after liver transplantation in a patient with HIV coinfection. It confirms that telaprevir-based triple therapy can be used to treat HCV recurrence in HIV patients, so long as they are monitored closely at a center with experience in transplanting HIV patients.
Telaprevir and boceprevir have revolutionized the treatment of HCV genotype 1 infection. Both medications are substrates and inhibitors of cytochrome P450 3A, which are important for the metabolism of many medications used to treat HIV. Therefore, neither drug is FDA-approved for use in liver transplant recipients or in patients coinfected with HCV and HIV, due to concerns about the potential for serious drug interactions. This patent was treated when telaprevir was the highest level of therapy for patients with HCV. Today, newer direct-acting agents can produce a response rate of 80 to 85 percent.
Cleveland Clinic gained a solid experience in managing immunosuppression regimens and drug-drug interactions while using protease inhibitors in prior transplant cases involving HIV-positive patients.
Regardless of the agent used, management of HCV-HIV coinfection in the context of post-transplant immunosuppression requires a collaborative team of hepatologists, virologists and transplant surgeons who recognize the critical need for vigilant monitoring in this setting.
Photo Credit: Centers for Disease Control and Prevention
Advertisement
Advertisement
Strong patient communication can help clinicians choose the best treatment option
ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance
The importance of raising awareness and taking steps to mitigate these occurrences
New research indicates feasibility and helps identify which patients could benefit
Treating a patient after a complicated hernia repair led to surgical complications and chronic pain
Standardized and collaborative care improves liver transplantations
Fewer incisions and more control for surgeons
Caregiver collaboration and patient education remain critical