Remote endarterectomy avoids third bypass operation
By W. Michael Park, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 67-year-old woman was referred for management of an infected femorofemoral bypass graft that had been placed for a left common iliac artery occlusion. Her surgeon resected the distal graft, packed the wound open and transferred the patient to Cleveland Clinic.
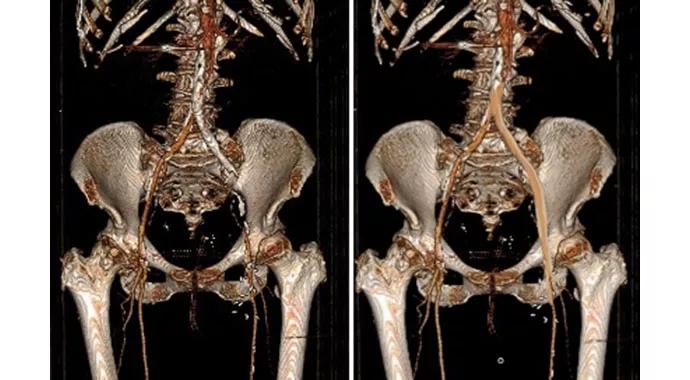
The patient had undergone prior left common iliac artery stent placement and femorofemoral bypass, both of which had occluded in the past year. Upon presentation, the patient was experiencing ischemic pain in the left leg at rest. A contrast CTA showed an occluded left common iliac stent and left external iliac artery. The remnant proximal redo femorofemoral graft was surrounded with fluid. The previous femorofemoral bypass appeared well incorporated.
Revascularization options included a third femorofemoral bypass reoperation using deep femoral vein versus cryopreserved artery. On review of the CTA, it appeared that revascularization of the native circulation using remote endarterectomy to remove the occluded stent and occlusive external iliac artery plaque was feasible, and this approach was chosen.

The patient’s left groin incision was reopened to gain control of the common femoral artery. Using a Vollmer ring dissector, the occluding left external iliac artery plaque was dissected up to and around the stent and, eventually, up to the origin of the iliac artery. A Moll ring cutter was then used to transect the heavily calcified plaque at the aortic bifurcation. This restored patency of the occluded left iliac system. The bifurcation was then treated with kissing iliac stents. The common femoral artery was patched with vein, and the wound closed with a sartorius muscle flap. The remnant femorofemoral bypass graft was easily removed from the right groin exposure and the artery repaired. This wound was also closed with a sartorius muscle flap.
Advertisement
Remote endarterectomy is a minimally invasive adaptation of an old and established revascularization technique.
Remote endarterectomy uses endovascular techniques and fluoroscopy to manage with a single incision a procedure that otherwise would require two or more incisions. It avoids prosthetic graft materials, making it ideal for infected graft cases.
In this patient, remote endarterectomy was possible because the common iliac stent was an undersized, balloon-expandable stent, which the Vollmer ring dissector easily accommodated. A larger stent would have precluded safe dissection.
Remote endarterectomy allowed us to avoid deep femoral vein harvest, which would have lengthened the operation and increased morbidity. Had remote endarterectomy failed, the option of deep femoral vein harvest and bypass remained available.
The patient’s right groin wound was closed in the hospital, and she was discharged home with a wound VAC on the left groin. At three-month follow-up, she had fully recovered.
Dr. Park is a vascular surgeon in the Heart & Vascular Institute with a specialty interest in minimally invasive treatment of vascular disease.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable