Dual heart and stem cell transplants reflect progress

In October 2013, a 65-year-old male physician from Dallas diagnosed with hypertrophic cardiomyopathy saw Cleveland Clinic heart failure specialist Mazen Hanna, MD, for a second opinion. The former marathoner had been treated for heart failure for about a year but was rapidly declining.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Finding the patient’s test results inconsistent with the diagnosis (Figure 1), Dr. Hanna ordered more-sensitive tests, which revealed cardiac amyloidosis (Figures 2 and 3) — specifically, AL amyloidosis — that was soon confirmed by biopsy. Chemotherapy was promptly started. The patient returned to Texas, and with a Cleveland Clinic hematologist coordinating his chemotherapy, he achieved very good partial remission.
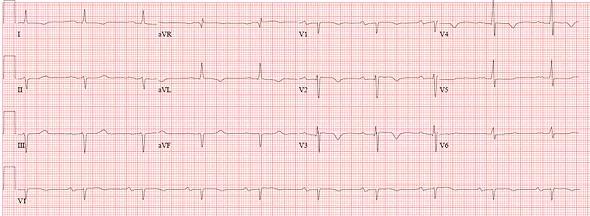
Figure 1. This ECG from the case patient does not meet low voltage criteria but shows relatively low voltage vs. what would be expected in a patient with severe left ventricular hypertrophic cardiomyopathy.
Despite an amyloidosis-specific cardiac care regimen, however, his heart failure worsened. Dr. Hanna proposed an aggressive treatment: heart transplantation followed by stem cell transplantation. The patient agreed. Through Cleveland Clinic’s cardiovascular clinical and research alliance with Baylor Scott & White Health in Dallas, he was listed for a heart transplant at Baylor in July 2014 and received a new heart five days later. Chemotherapy was continued during his recovery. In February 2015, he underwent an autologous stem cell transplant at Cleveland Clinic. Within a few months, he was in complete remission, had returned to work full time and had resumed running.
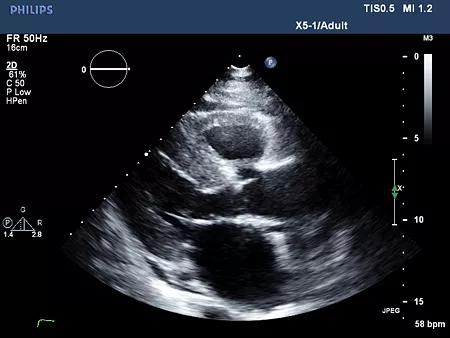
Figure 2. Echocardiogram of the case patient (parasternal long axis view) showing diffuse thickening of the left and right ventricular walls.

Figure 3. Photo of the case patient’s explanted heart. Note the dramatic thickening of all chambers, which is typical of cardiac amyloidosis.
Advertisement
Cleveland Clinic is one of the few U.S. centers offering heart and stem cell transplantation for selected patients with cardiac amyloidosis. The treatment approach is emblematic of a commitment to changing the outlook for patients with this formerly incurable disease.
“The prognosis for cardiac amyloidosis is not hopeless,” says Dr. Hanna. “Once diagnosed, however, it requires significant expertise to treat. A multidisciplinary team like the one we have here is an enormous asset.”
Amyloid deposits can occur in any organ in the body. Approximately 50 new patients with cardiac involvement are among those seen in Cleveland Clinic’s Amyloidosis Center every year. The center includes specialists from multiple disciplines — cardiology, hematology-oncology, nephrology, neurology, gastroenterology, pathology, transplantation and palliative care — who meet bimonthly to discuss cases.
Of the patients with cardiac amyloidosis, about 40 percent have light chain amyloidosis due to a plasma cell dyscrasia (AL amyloidosis) and 60 percent have transthyretin-related (TTR) amyloidosis. “The distinction is critical,” says Dr. Hanna, “because the two forms require very different treatments.”
AL amyloidosis is a rapidly progressing, life-threatening disease. Several types of chemotherapy, used with or without transplantation, are reserved for this form. Cleveland Clinic is taking part in clinical trials of NEOD001, a humanized monoclonal antibody designed to potentiate the effects of chemotherapy against AL amyloidosis. “We’re excited about the potential of this biologic, which may clear existing amyloid deposits,” Dr. Hanna notes.
Advertisement
For patients with TTR amyloidosis, investigational drugs are showing promise in slowing disease progression. Cleveland Clinic offers participation in clinical trials of two such agents:
Knowledge about cardiac amyloid disease is being advanced at Cleveland Clinic by a $2 million gift in 2014 from an anonymous donor. Dr. Hanna is using the funds to support research projects and a research fellow dedicated to the subspecialty.
These developments reflect growing interest in the disease among Cleveland Clinic cardiologists and colleagues in other specialties. “We have two cardiology fellows specializing in amyloid, and all our cardiologists are invested in the condition,” says Dr. Hanna. “As a result, amyloidosis is being diagnosed with increasing frequency.”
And when patients are diagnosed with amyloidosis in other organs, Dr. Hanna — who directs cardiac amyloidosis care at Cleveland Clinic — is routinely asked to screen them for cardiac involvement.
Therapy addresses both HF and underlying amyloid disease
Once cardiac amyloidosis is identified, early referral to a center with experience treating it is not only recommended — it may be lifesaving.
“Treatment is generally complex and requires managing the patient’s heart failure while treating the underlying disease,” Dr. Hanna explains. “Amyloid patients cannot be treated like other heart failure patients. It’s as important to know what not to give them as what to give them, since many common heart failure drugs will be poorly tolerated or detrimental, and patients may not respond to medications as expected.”
Advertisement
For patients with AL amyloidosis, an individualized, aggressive chemotherapy regimen must be initiated to stop production of abnormal light chains in the plasma. Individual patients may be candidates for additional therapy with stem cell transplantation. Some patients may be candidates for heart transplantation, which can be considered in highly selected AL amyloidosis cases with advanced cardiac amyloid without severe involvement of other organs.
For some patients with TTR amyloidosis, heart transplant or combined heart and liver transplant may be feasible. “Thus far, we have performed seven heart transplants in these patients, one with combined liver transplant,” Dr. Hanna notes. “All have had very good outcomes.”
According to Dr. Hanna, cardiac amyloidosis is not rare; it is underdiagnosed. He says any of the following findings should prompt a high index of suspicion for amyloidosis:
He recommends screening for a monoclonal process with serum free light chain assay (kappa and lambda) and serum and urine immunofixation. He advises against ordering routine serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) when cardiac amyloidosis is suspected. “They are not sensitive enough; even when results are negative, a patient can have AL amyloidosis.”
Patients whose lab tests show no monoclonal protein can still have TTR amyloidosis. Imaging techniques such as cardiac MRI, echocardiography (Figure 2) with longitudinal strain analysis, and technetium pyrophosphate scanning are noninvasive workup methods. Definitive diagnosis is made by endomyocardial biopsy.
Advertisement
Cleveland Clinic cardiologists collaborate with amyloidosis centers at other institutions to improve outcomes for patients of all ages with the disease. The clinicians and researchers have monthly conference calls and meet yearly with patients and families. “It’s all about helping each other fight this disease,” Dr. Hanna says.
He is encouraged by rapid progress in all areas of diagnosis and treatment. “When I started in medicine, we saw so many patients with no options. Now this area of cardiology is progressing and expanding.”
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable