Kidney failure, severe HTN call for a complex endovascular strategy
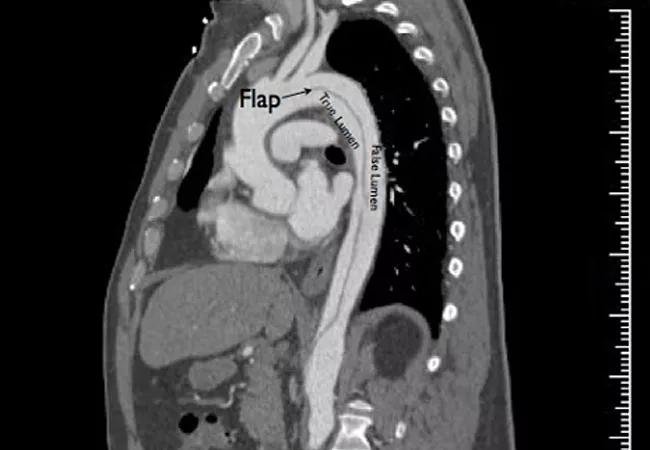
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/96d86b60-a7db-4e43-a9ae-2596e54288cd/16-HRT-1024-TypeB-Aortic-Dissection-CQD-650x450_jpg)
16-HRT-1024-TypeB-Aortic-Dissection-CQD-650×450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 51-year-old man with a history of difficult-to-control hypertension and smoking presented to an outside institution with severe chest pain associated with shortness of breath.
His blood pressure was 248/119 mmHg. CT revealed a descending thoracic aortic dissection (Figure 1). He had acute renal failure with an elevated creatinine that peaked at 2.4 mg/dL. His hypertension was eventually controlled on a five-drug regimen (clonidine, losartan, carvedilol, hydralazine and amlodipine). Despite this, his systolic pressure remained persistently above 160 mmHg and he had persistent back pain. His renal function stabilized at a creatinine of 1.8 mg/dL, indicating that he had lost almost half of his baseline kidney function.
He was going to be discharged for medical management of his aortic dissection, but he requested a second opinion and was transferred by air to Cleveland Clinic.
On arrival here, his systolic blood pressure remained above 160 mmHg and he continued to report back pain. Review of his prior CT (Figure 1) revealed compression of most of his true lumen, compromising flow into the kidneys, which were perfused by the false lumen. He also had diminished lumen flow into his abdominal viscera (stomach, liver, intestines) and legs, although he remained asymptomatic in these vascular beds.
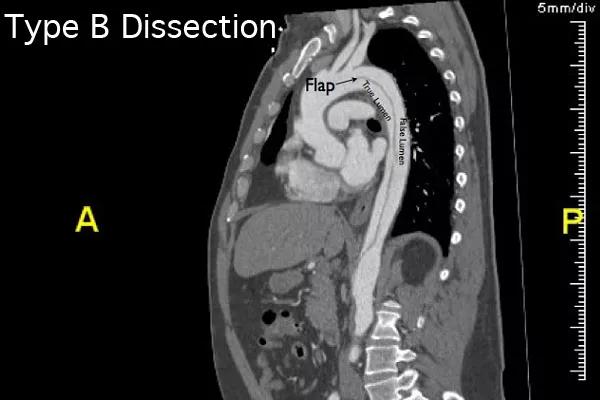
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/60e984e7-63a1-4dd9-b2fd-0e12281ec38f/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-1_jpg)
Figure 1. The patient’s CT at presentation.
His continued back pain concerned me because it could herald eventual rupture if his blood pressure remained high. This was a long-term consideration as well, and his relatively young age meant he’d be likely to suffer the side effects of taking so many blood pressure medications — including lethargy, depression and impotence.
Advertisement
A plan was made to operate (Figure 2), with the goal of re-establishing true lumen flow by closing off the proximal entry point and supporting the true lumen to allow it to fully re-expand. This was to be done with a thoracic stent graft sized appropriately for the total size of the aortic adventitia. As hybrid stent graft/stent devices for dissection are not commercially available in the U.S., an available stent graft was chosen to cover the proximal dissection. Any residual stenosis in the renal or other arteries would be treated with stenting from the true lumen. This would allow for reperfusion of the kidneys, with the goal of better blood pressure control and kidney function. Incidentally, the size of his femoral and iliac arteries was suitable for a total percutaneous repair.
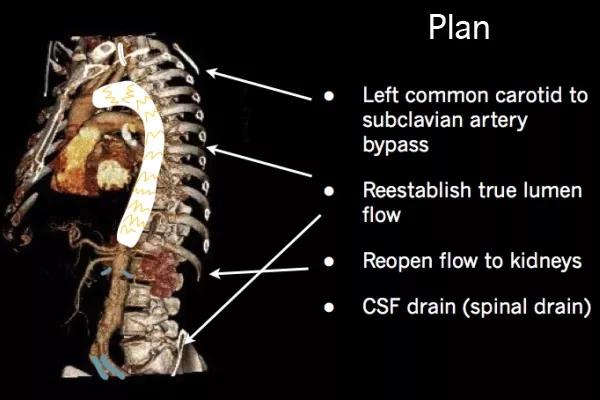
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3a040db7-426d-4892-84cb-24a0450c4246/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-2_jpg)
Figure 2. The operative plan.
Because the dissection started next to the left subclavian artery, the thoracic stent graft to be placed to seal the proximal start point of the dissection would cover the left subclavian artery orifice. A bypass from the left common carotid artery to the left subclavian artery was planned to avoid loss of flow to the left hand and, crucially, to the left vertebral artery to the brain.
After bypass of the left common carotid artery to the left subclavian artery, the patient was re-prepped and both common femoral arteries were accessed under ultrasound.
B-mode ultrasound showed a single lumen to the common femoral arteries, suggesting that the dissection had not extended to the groins and that true lumen access would be possible. Wire access was achieved up to the aortic arch and intravascular ultrasound (IVUS) was used to confirm that the wires were in the true lumen (Figure 3).
Advertisement
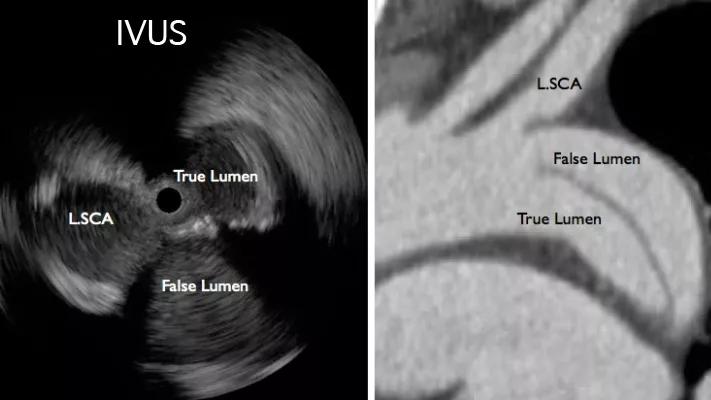
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a9a2add7-3d0a-4653-9072-85014cb4c23a/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-3_jpg)
Figure 3. Intravascular ultrasound confirmed the wires were in the true lumen.
A thoracic stent graft (Gore TAG®) was deployed across the origin of the left subclavian artery to seal off the origin of the false lumen flap (Figure 4) and extended to the thoracic aorta above the celiac axis.
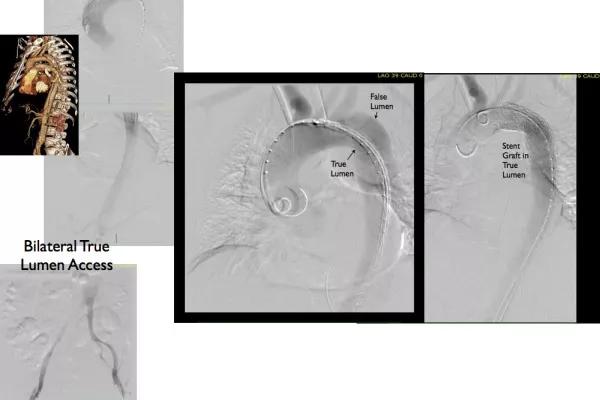
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56464883-d2ad-4dfd-aac2-3ea3d1860b5b/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-4_jpg)
Figure 4. Deployment of the thoracic stent graft.
IVUS confirmed re-establishment of true lumen flow into the visceral segment of aorta. Selective renal arteriography showed stenoses due to the false lumen flaps, which were treated with stents (Figure 5). The flap impinged on iliac flow by IVUS and arteriography, and this area was stented (Figure 6). The arterial access sites were repaired with pre-placed Perclose sutures.
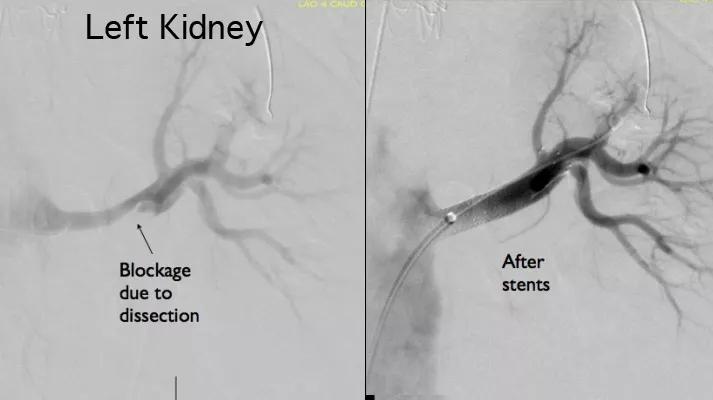
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1370d816-4950-4a7c-a9b4-b8cef88ccc89/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-5_jpg)
Figure 5. Renal arteriographs showing blockage before surgery (left) and the result of the surgical repair (right).
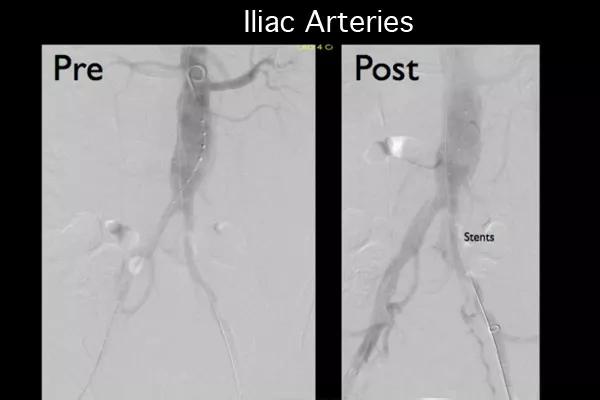
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/129ae498-262c-47bd-87a4-02a3b7ff333e/16-HRT-1024-TypeB-Aortic-Dissection-CQD-Inset-6_jpg)
Figure 6. The iliac arteries before (left) and after (right) the procedure.
The patient recovered well and demonstrated excellent blood pressure response, with systolic pressures at discharge in the vicinity of 120 mmHg on four medications, which were reduced to three after discharge. Gratifyingly, his pain remitted and his renal function improved, with creatinine levels decreasing from 1.8 mg/dL on admission to 1.46 in the operating room and gradually down further to 1.18 mg/dL on postoperative day 3.
While there are theoretical benefits to endovascular treatment of type B thoracic aortic dissection, the randomized INSTEAD trial (Circulation. 2009;120:2519-2528) failed to prove a difference in two-year survival between medically managed and stent-grafted groups, but the aortas in the stent-grafted group had better remodeling.
Advertisement
When thoracic endografting and endovascular therapy is used to treat malperfusion, there is an early mortality rate of 2.8 to 16 percent, a stroke rate of 1.5 to 9.5 percent, and a paraplegia rate of 0 to 2.8 percent (DiMusto et al, J Vasc Surg. 2010;52[4 suppl]:26S-36S). There is likewise is a risk of retrograde dissection (and conversion to type A dissection) of 1.9 percent and a reintervention rate of 7.6 percent. The long-term results are unknown.
That said, in carefully selected individuals with good anatomy, and with the right equipment, successful outcomes are possible.
Dr. Park (parkm3@ccf.org) is a vascular surgeon in Cleveland Clinic’s Miller Family Heart & Vascular Institute.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable