Reflections following one of the device’s first placements in the U.S.

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Early-onset scoliosis remains one of the most therapeutically challenging entities encountered by the pediatric spine deformity surgeon. Children with severe deformities are often treated with some sort of early nonfusion intervention in an attempt to control the deformity until the chest cage grows large enough to accommodate the child’s growing lungs into adulthood.
When intervention is required, it often consists of a growing rod construct designed to serve as an internal brace and support the corrected spine without fusion. Unfortunately, these static devices require repeat surgical lengthening roughly every six months to accommodate the child’s growing spine from the time of implantation until definitive fusion is accomplished once the chest cage has matured sufficiently — typically at age 10 to 12. This creates a huge burden of morbidity and cost.
Fortunately, a less-burdensome alternative emerged with the 2014 FDA approval of a novel spine implant from Ellipse Technologies called the MAGEC® (Magnetic Expansion Control) System, which allows the growing rod construct to be lengthened nonsurgically in the office. Use of a magnetic actuator applied to the patient’s skin allows painless lengthening of the construct at the frequency and magnitude desired by the surgeon.

Photos of Dr. Goodwin with the recipient of the first magnetic growing rod implanted at Cleveland Clinic, taken at a post-implantation follow-up visit. In the first photo, the patient’s back is marked to guide placement of the magnetic growing rod’s magnetic actuator on the skin (second photo) to enable painless lengthening of the rod in the office.
Advertisement
This technology has the ability to significantly reduce the number of revision operations children with severe early-onset scoliosis require to treat their deformities. Its potential is illustrated by the index case for placement of the magnetic growing rod at Cleveland Clinic, a boy with infantile idiopathic scoliosis who was among the first U.S. recipients of the device following its FDA approval.
The patient initially had a traditional growing rod placed at age 2 years for a spinal deformity of greater than 90 degrees. He later developed an infection after one of several traditional rod-lengthening surgeries. Removal of all implants was required to eradicate the infection. When the patient was re-instrumented, the MAGEC device was used. He was 5 years old when it was placed in autumn 2014.
The patient has since undergone three lengthenings of the device, all performed noninvasively in the office using the device’s magnetic actuator (see images above). The correction has been maintained thus far, and the boy has reported no pain or neurologic complaints during or after the lengthenings.
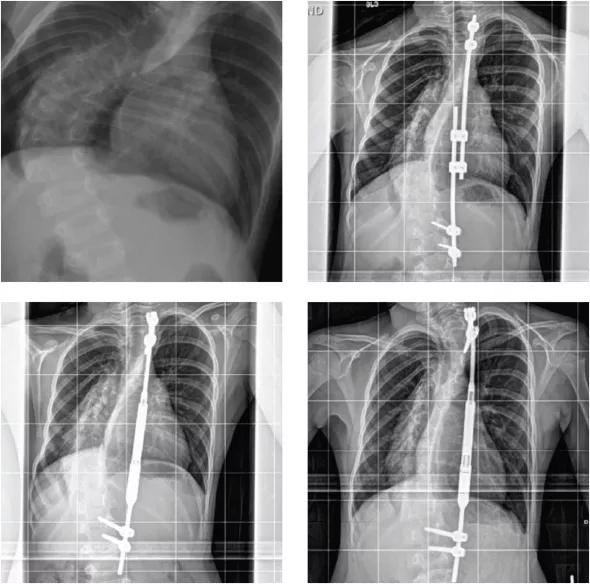
Posteroanterior radiographs of the boy with infantile idiopathic scoliosis who received the first MAGEC magnetic spinal growing rod at Cleveland Clinic. Top left: Image of the patient’s severe early-onset scoliosis at age 2 years, prior to surgical intervention. Bracing and casting had failed to control the deformity. Top right: Two years after placement of traditional growing rod instrumentation, prior to infection and the rod’s removal. Bottom left: Following placement of the magnetic growing rod in autumn 2014. Bottom right: After lengthening of the magnetic growing rod in the office. Note the expansion of the rod’s central barrel.
Advertisement
This device appears to be a safe alternative to traditional growing rod constructs and has the potential to avoid substantial morbidity and achieve considerable overall cost savings by significantly reducing the number of lengthening surgeries. Future studies on its more widespread use should shed light on the full impact this technology will have in this challenging patient population.
Dr. Goodwin is Director of the Center for Pediatric Orthopaedic Surgery. His specialty interests include scoliosis and spinal deformity.
Advertisement
Advertisement

Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients

How to diagnose and treat crystalline arthropathy after knee replacement

Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network

Reduced narcotic use is the latest on the list of robotic surgery advantages

Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals

Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions