Tailor essential features and functions to your needs

By Rishi P. Singh, MD, Cleveland Clinic Cole Eye Institute vitreoretinal surgeon
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Good features can significantly smooth the bumpy road to the adoption of a medical records system.
Adding customized, intuitive functions can improve your work flow and practice efficiency. When Cleveland Clinic’s Cole Eye Institute first made the transition to EMR, our group spent several months evaluating several systems to find just the right tools.
Even if specific capabilities weren’t initially within the system, we worked with the vendor and our IT people to create and implement those special features. These can be broken down into three distinct groups: improving the user experience of both providers and support staff; improving the billing capture and process; and integrating outcomes, administrative tasks and research activities.
Ergonomics is a key element in facilitating user adoption and acceptance of any EMR system. By incorporating the largest monitors possible, we were able to distribute a significant amount of information across a larger space. A couple key factors of the system have made it easier for physicians to adapt to the new EMR work flow:
Drawing is a mainstay of ophthalmology practices. We have created newer pictures to represent the portions of the eye that require documentation. Creating numerous stencils for each of the drawing photos eliminates duplication of work and allows for:
Advertisement
We also improved the letter-writing and documentation capabilities of our system:
By using the discrete elements within our system, we created additional data streams that determine a multitude of administrative and research functions.
The number of procedures and diagnostics in ophthalmology has drastically increased over the past few years. Take for example the use of intravitreal injections for eye disease. In the past five years, the number of times that procedure is done has quadrupled. Increased volume has made it difficult to track procedures and submit charges in an efficient fashion.
Our new charge-on-completion system offers:
Here’s how it works:
This has streamlined our billing cycle from weeks to two days. It’s also decreased the potential for miscoding since it has completely eliminated manual entry. Finally, it allows for a transparent review of the indication and necessity of the procedure.
Advertisement
Since 2005, all Cleveland Clinic institutes have participated in a patient outcomes reporting initiative. Until recently, the outcomes data has been compiled using manual entry and physician reporting, both ways by which reporting biases could be introduced. When we developed the entry system for our EMR, a conscious effort was made to use discrete documentation whenever possible. For example, few areas in the system have plain-text boxes for entry. Rather, buttons and checkboxes are used to document imaging, procedures and exam elements. This allows us to collect outcome metrics in an almost completely automated fashion. In addition, by using the discrete elements within our system, we created additional data streams that determine a multitude of administrative and research functions.
Overall, these features have allowed for the ongoing evaluation and management of the physician and patient experience and will lead to future enhancements of both functions.
Advertisement
Advertisement
Early data shows risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis

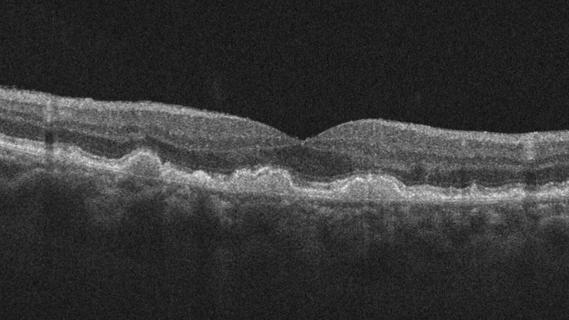
Identifies weak spots in the cornea before shape change occurs

Study highlights the value of quantitative ultra-widefield angiography

Switching medications may decrease treatment burden and macular fluid

Interventions abound for active and stable phases of TED

Corneal imaging and interpretation play a major role

Cole Eye Institute imaging specialists are equal parts technician, artist and diagnostician

Effect of low-dose atropine and dual-focus contact lenses is unknown in patients with comorbid eye conditions