Case study in how echo labs can enhance CQI processes

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/49748952-a080-4494-96e8-049aefde6e5f/18-HRT-311-Valley-Health-CQD-Hero_jpg)
18-HRT-311-Valley-Health-CQD-Hero
For echocardiography laboratories, a standardized continuous quality improvement (CQI) program is essential, as quality assessment and improvement strategies are critical to ensuring accuracy and reproducibility of echocardiography procedures. Although echo lab CQI programs are recommended by both the Intersocietal Accreditation Commission and the American Society of Echocardiography, adoption of a CQI plan is left to the discretion of individual echo labs, with no formal industry standardization and no required measures to evaluate performance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The CQI program for Valley Health System’s echocardiography lab was limited when the Ridgewood, New Jersey-based health system became an affiliate of Cleveland Clinic’s Miller Family Heart & Vascular Institute in January 2017. Review and enhancement of affiliate organizations’ CQI programs is an important component of services offered by Cleveland Clinic’s Heart & Vascular Institute Affiliate Program, and CQI in the echo lab was a priority for Valley Health System.
Early in the affiliation, key players from Cleveland Clinic’s Section of Cardiovascular Imaging performed quality assurance (QA) on a portion of transthoracic and transesophageal echocardiograms for Valley Health System. The peer-to-peer review was designed to provide a baseline quality assessment for Valley Health System’s echo lab and offer recommendations for enhancements to the image and reporting capabilities. Peer-to-peer outcomes were provided through written formal feedback and conference calls between Valley Health System’s cardiovascular imaging team and three Cleveland Clinic cardiovascular imaging specialists — Richard Grimm, DO; Brian Griffin, MD; and Suma Thomas, MD — as well as Cleveland Clinic consulting cardiac sonographer Kimberly Radigan, RDCS.
The QA process typically involves exposing the affiliate program to Cleveland Clinic’s internal echocardiography CQI program, to demonstrate the feasibility of a standardized, routine and structured peer-review process that has been incorporated into daily operations at a large tertiary referral hospital. The process is centered on constructive feedback and includes both sonographers and physician readers, with the goal of improving consistency in image acquisition by the sonographer and interpretation by the physician.
Advertisement
Cleveland Clinic’s echocardiography CQI program has been in place for approximately five years. It is consistent and well-accepted and has proven feasible despite a relatively high volume of studies performed. Each business day, 2 to 5 percent of the completed echocardiographic studies are randomly selected for review. Experienced sonographers and readers perform the reviews, reporting their level of agreement/disagreement based on predefined fields. In cases of disagreement, the original sonographer/reader is notified. This process is followed up with monthly quality meetings at which sonographers and physicians participate in reviewing quality outcomes.
The peer-review process evaluates the technical quality of the images acquired and the interpretive accuracy of the reading physician. The percent agreement in the sonographer review process has been increasing with time in key areas — for example, agreement on contrast use rose from 83 to 97 percent. Similarly, the percentage of “no disagreements” in the reader review process has increased — from 50 to 62 percent — over the same period.
At the end of the QA review, the Cleveland Clinic team proposed a feasible peer-review process that could serve as the platform for a structured CQI program for the Valley Hospital echo lab. Valley Hospital adopted the proposal, much of which was adapted from Cleveland Clinic’s CQI program, and has continued to embrace quality improvement projects.
Implementation of the new process at Valley Hospital has met with considerable success. The imaging management team reports increased communication among physicians as well as between sonographers and physicians. Likewise, educational and quality meetings have been expanded in scope and increased in frequency to a monthly basis. Establishment of a physician-led peer-review process has reduced reporting discrepancies (Figure 1). The imaging management team has followed through on recommendations to revise the standard comprehensive protocol while sonographers have enhanced and optimized equipment capabilities. The protocol and metrics set in place were derived from the initial feedback from Cleveland Clinic, but the driving forces behind the accomplishments outlined above have been Valley Medical Group physicians Michael Anshelevich, MD, and Howard Goldschmidt, MD, and the Valley Hospital echo lab management team.
Advertisement
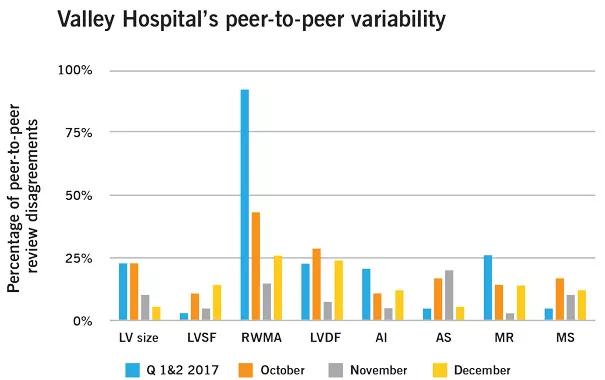
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/27f6aa87-4728-4e00-8b64-7304fd6f664d/18-HRT-311-Valley-Health-CQD-chart-003_jpg)
Figure 1. Graph showing peer-to-peer variability in echocardiogram reviews before and after Valley Hospital’s adoption of Cleveland Clinic’s CQI program recommendations in the third quarter of 2017. LV = left ventricular; LVSF = LV systolic function; RWMA = regional wall motion abnormalities; LVDF = LV diastolic function; AI = aortic insufficiency; AS = aortic stenosis; MR = mitral regurgitation; MS = mitral stenosis.
To build on this success, Valley Hospital’s echo lab management team collaborates monthly with Cleveland Clinic’s imaging consultant to discuss the lab standards and areas of opportunity. Strategies to ensure quality metrics are discussed, along with innovation, educational opportunities and changes in American Society of Echocardiography guidelines. Innovative methodologies, such as myocardial deformation (strain), 3-D acquisition, and ultrasound enhancement agents, are highlighted topics of interest.
“The genesis of our new quality process is based on guidelines and recommendations shared by Cleveland Clinic during our assessment,” says Stacy Mack, MBA, Assistant Vice President, Heart and Vascular Institute, Valley Health System. “We have further reinforced the quality and improvement initiatives by incorporating two physician co-directors to oversee the process with Cleveland Clinic’s support.”
“Valley Hospital has truly embraced and leveraged its affiliation with our Heart & Vascular Institute and has consequently seen positive outcomes in both image acquisition and physician reporting, resulting in improved patient care,” observes Dr. Richard Grimm, Director of Echocardiography Laboratories, Cleveland Clinic.
Advertisement
For details on affiliation opportunities with Cleveland Clinic’s Heart & Vascular Institute, visit ahsproviders.com.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable