Most patients report relief from intractable spasms

Chemodenervation therapy using botulinum toxin offers a low-risk option for often painful and disabling movement disorders that are difficult to treat. Success rates for improving symptoms merit trying this treatment before embarking on a surgical course of action.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Outcomes data from the use of this strategy in Cleveland Clinic’s Center for Neurological Restoration in 2015 reveal that a variety of difficult-to-treat movement disorders are amenable to improvement. Injected directly into involved muscles, botulinum toxin (Botox®, Dysport®, Myobloc® and Xeomin®) tends to be most effective in treating spastic disorders involving only a few muscle groups. Most patients require repeat injections every three to four months as the effects of the toxin wears off.
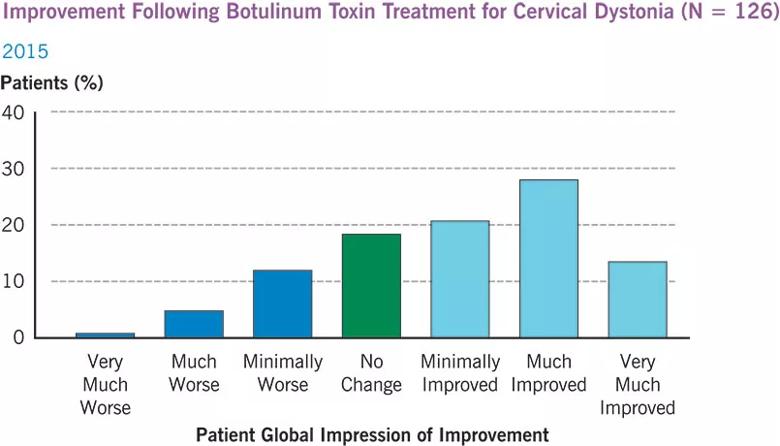
Of the 126 patients treated with botulinum toxin in 2015 at Cleveland Clinic for cervical dystonia (spasmodic torticollis) — most of whom had complex presentations — 62 percent rated their condition as improved on the Patient Global Impression of Improvement (PGI-I) questionnaire (see table below). This response rate was achieved despite the high acuity of patients and the fact that a significant portion of cases had failed to respond to botulinum toxin injections from other providers. Fewer than 20 percent of patients rated their condition as worse following treatment, with most rating it as minimally worse.
Other movement disorders, including other forms of dystonia, hemifacial spasm and spasticity, can also be treated with botulinum toxin, as can intractable migraine.
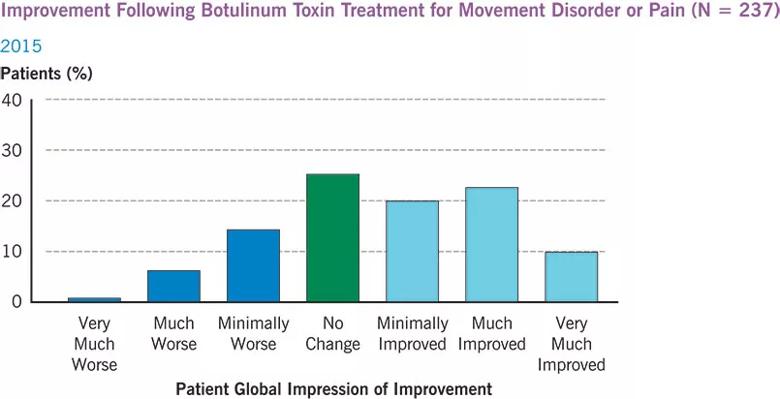
Out of all patients treated with chemodenervation at Cleveland Clinic in 2015 (N = 237), including those with medication-resistant migraine, hemifacial spasms and dystonia, more than half (53 percent) rated their condition as improved on the PGI-I questionnaire (see table below). Of the approximately 20 percent who reported their condition as worse, most rated the worsening as minimal.
Advertisement
Cleveland Clinic systematically collects and reports quality and outcomes measures for other treatments for movement disorders, including spinal cord stimulation and deep brain stimulation. These data, as well as outcomes for the full range of neurological disorders treated at Cleveland Clinic, can be accessed online in the 2015 Neurological Institute Outcomes Book.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade