Recognizing and supporting diabetic patients

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

Cecilia Lansang, MD, MPH
As endocrinologists, your patients with diabetes may be hospitalized for a variety of reasons, including cardiovascular, gastrointestinal or other disease. At Cleveland Clinic’s Endocrinology Consult Service, we help balance patients’ autonomy and safety as they navigate their hospital stay.
At Cleveland Clinic, at least 50 patients using an insulin pump were admitted last year, and more and more patients are choosing this option for managing their diabetes. This continuous subcutaneous insulin infusion (CSII) method of delivery allows patients to self-manage and affords them flexibility suited to their lifestyles.
When patients on insulin pumps are ill and hospitalized, however, they may need assistance with adjusting insulin doses, or may need to be switched to basal-bolus subcutaneous insulin injections if they are unable to continue to care for themselves. Therefore, physicians and other inpatient providers must be able to recognize these patients in the hospital, make the decision to continue the pump and guide patients regarding dose changes, or discontinue the pump with an appropriate change to basal-bolus insulin.
The American Diabetes Association and American Association of Clinical Endocrinologists advocate for allowing patients who are physically and mentally able to continue CSII when hospitalized, and recommend that hospitals establish an appropriate policy and make available hospital personnel with expertise in pump management. Cleveland Clinic has such a policy, and strongly encourages an endocrinology referral for subspecialty partnership in taking care of these patients.
Advertisement
Here are highlights of the basics that we share with other providers:
General contraindications to insulin pump use in the hospital:
Once patients requiring inpatient insulin pump therapy are identified, insulin pump orders must be issued to ensure that insulin is delivered to them from the pharmacy, to have their point-of-care glucose readings taken, and to receive assistance with dosing or carbohydrate counting.
If the decision has been made to discontinue an insulin pump while in the hospital, patients are often best managed on a long-acting insulin for basal needs, mealtime insulin to cover the carbohydrates in the meals and supplemental insulin to correct for hyperglycemia.
Advertisement
Cecilia Lansang, MD, MPH, is Director of Inpatient Diabetes Services in the Department of Endocrinology, Diabetes and Metabolism at Cleveland Clinic and an Associate Professor of Medicine at Cleveland Clinic Lerner College of Medicine. She can be contacted at 216.445.5246 or lansanm@ccf.org.
Advertisement
Advertisement
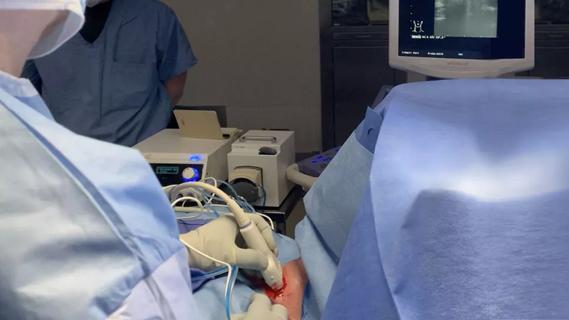
Radiofrequency ablation significantly reduces symptom severity, shrinks nodules

Maternal-fetal medicine specialists, endocrinologists and educators team up

Giving young patients a hand as they take charge of their own health

Case illustrates how easily condition can mimic preeclampsia
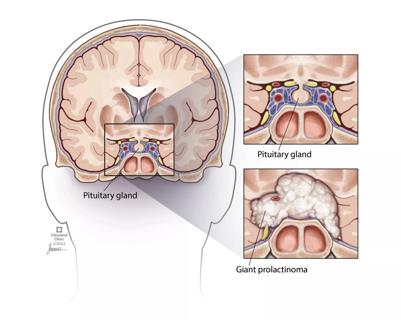
Analysis examines surgical resection of rare pituitary tumors
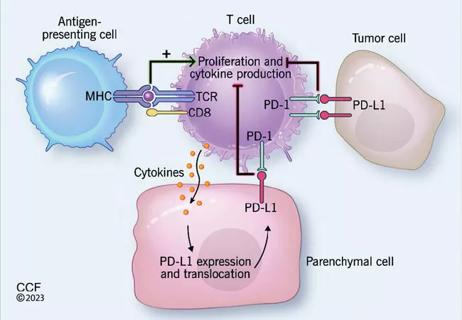
Screening and medication key to better outcomes

Spinal cord stimulation can help those who are optimized for success
Incidence, outcomes and management