Aflibercept dosing schedule works best

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Two important Phase 3 studies (VIEW 1 and VIEW 2) showed us that outcomes are similar for most patients with wet age-related macular degeneration if they undergo one of three treatment regimens: a 2 mg dose of intravitreal aflibercept (Eylea) injection either every four or eight weeks after three initial monthly injections, or 0.5 mg of ranibizumab (Lucentis) every four weeks after the initial dosing.
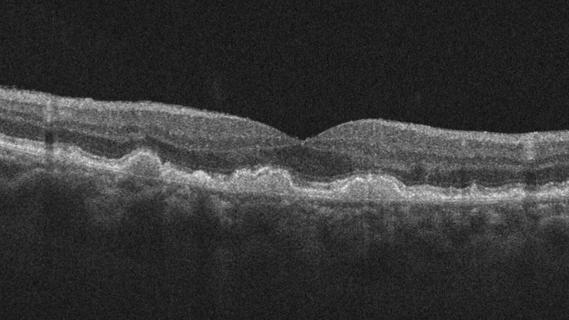
However, in these studies, as well as in the Comparison of Age-related Macular Degeneration Treatment Trials (CATT) study, a small subgroup of eyes continued to have residual intraretinal fluid present despite treatment, and this correlated with worse visual acuity.
Our group of investigators sought to learn which dosing regimen was the best way to approach treating these patients, and I am pleased to report that we did indeed identify a best practice: giving aflibercept monthly yields significantly better outcomes than either of the other two protocols.
Our post hoc analysis of eyes enrolled in VIEW 1 and VIEW 2 reviewed the data from 815 eyes with wet AMD and known fluid status at baseline and weeks four, eight and 12 in all three treatment groups. Outcome measures that we studied included mean best-corrected visual acuity (BCVA) change from baseline over weeks 16 to 52 and the proportion of eyes that gained or lost at least five letters. We reviewed eyes with and without persistent fluid (cystic intraretinal or subretinal fluid at all four initial visits), and broke down the findings by fluid type.
Advertisement
The percentage of eyes with persistent fluid was 29.4 in the ranibizumab 0.5 mg every four weeks group, 18.8 in the 2 mg of aflibercept group, and 20.3 in the 2 mg of aflibercept every eight weeks group. In these eyes, mean BCVA gain from baseline to week 52 was greatest in the 2 mg of aflibercept every four weeks group. The other two groups were found to have outcomes that were similar to one another. The outcomes did not vary by the type of fluid that was present. In eyes without persistent fluid, BCVA changes were similar across the treatment groups.
These were not surprising findings. This difference in this subgroup of difficult-to-treat patients was suggested by other studies, since aflibercept dried the retina better than ranibizumab.
At the Cole Eye Institute, we typically have started our wet AMD patients on bevacizumab (Avastin) and if they were not improving adequately, switched them to aflibercept or ranibizumab. With these findings, we are now much more likely to choose monthly aflibercept injections for eyes that continue to have persistent leakage.
Dr. Kaiser was the principal investigator for this study and also was on the study’s executive committee. He is the Chaney Family Endowed Chair of Ophthalmic Research and staff at Cole Eye Institute.
Advertisement
Advertisement
Early data shows risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis

Identifies weak spots in the cornea before shape change occurs

Study highlights the value of quantitative ultra-widefield angiography

Switching medications may decrease treatment burden and macular fluid

Interventions abound for active and stable phases of TED

Corneal imaging and interpretation play a major role

Cole Eye Institute imaging specialists are equal parts technician, artist and diagnostician

Effect of low-dose atropine and dual-focus contact lenses is unknown in patients with comorbid eye conditions