The case for a minimally invasive robotic approach to this form of mitral valve disease
Minimally invasive robotic, nonresectional mitral valve repair using neochords in Barlow’s disease is safe, effective and durable. That’s the consensus among Cleveland Clinic cardiothoracic surgeons, who are now using the technique on a regular basis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The technique avoids the fibrosis and scarring caused by extensive cutting and suturing,” says one of those surgeons, Per Wierup, MD, PhD. “It results in a larger opening with a lower gradient.”
The procedure can be completed more quickly with a robotic approach than a conventional repair performed with a sternotomy. “Patients tolerate it very well,” Dr. Wierup notes. “They require much less inotropic support and routinely only stay overnight in the ICU. Typically they can be discharged from the hospital after a few days.”
Barlow’s disease is one of two types of degenerative mitral valve disease causing mitral regurgitation, the other being fibroelastic deficiency. In contrast to the leaflet and chordal thinning seen in fibroelastic deficiency, Barlow’s is characterized by a large valve with redundant tissue that causes the valve to appear thick and swollen (Figure). A dilated annulus and elongated chords cause the entire valve structure to prolapse into the left atrium.
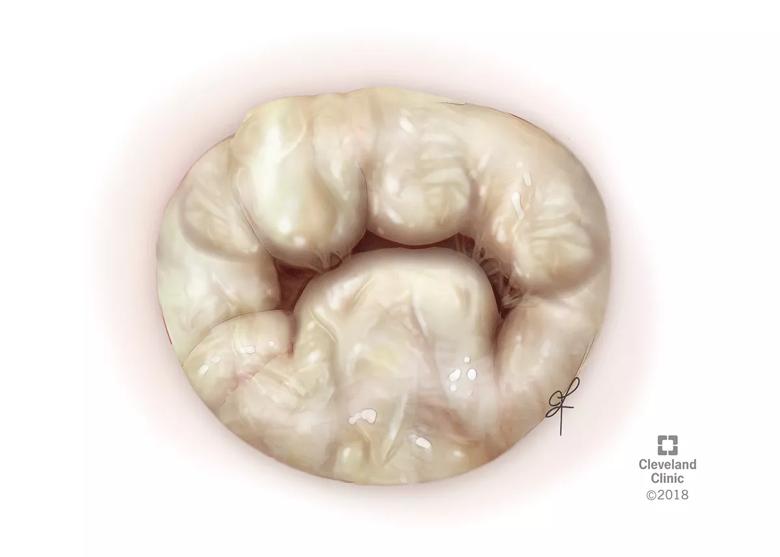
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f27061f8-b711-4ef1-acfc-eec5c816105f/19-HRT-080-Weirup-Barlow-inset_gif)
Figure. Illustration of a representative Barlow’s disease mitral valve with generalized thickening and redundant leaflet tissue.
Surgical correction of the regurgitation in Barlow’s disease offers a survival benefit when compared with optimal medical therapy or valve replacement. Conventional repair techniques used for fibroelastic deficiency have been problematic, however.
“In a conventional repair, the prolapsed sections of the valve are resected,” Dr. Wierup says. “A chordal transfer may be performed, and the remaining valve is reattached.”
Advertisement
More than a decade ago, Dr. Wierup began exploring how to improve on nonresectional techniques for Barlow’s disease. The approach treats the chords while leaving the leaflets intact.
“Leakage is caused by valve prolapse due to elongated chords, so we replace these with GoreTex® neochords,” he explains. “Making the chords on the anterior and posterior leaflets different lengths allows the zone of coaptation to be adjusted for perfect results.”
Performing the procedure using a minimally invasive, video-assisted robotic technique offers multiple advantages over conventional sternotomy, as demonstrated by outcomes from a recent retrospective review of 102 patients who underwent repair of Barlow’s disease. The results, which Dr. Wierup presented at the 2018 American Heart Association Scientific Sessions last November, included the following:
Advertisement
“Since he joined the Cleveland Clinic staff in 2017, Dr. Wierup has shared his techniques with other members of our mitral valve team, increasing the options we make available to treat patients with complex mitral valve disease,” says A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic.
“Minimally invasive repair using robotic assistance is now standard treatment for Barlow’s disease at our institution,” Dr. Wierup notes. “Patients must have a healthy aortic valve and groin blood vessels that are large enough to accommodate the cannulas required for robotic surgery. If their aortic valve is leaking, or their groin vessels are too small, it is safer to perform the repair using a minimally invasive alternative approach. However, this is necessary in only a minority of patients.”
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable