Cleveland Clinic experience demonstrates viability in a high-risk population

Of 21 consecutive patients with refractory ventricular tachycardia (VT) in cardiogenic shock, most (81%) could be successfully weaned off mechanical support following radiofrequency ablation. So reports a group of Cleveland Clinic clinicians in an analysis published in Circulation: Arrhythmia and Electrophysiology. All of the patients had previously been unable to be removed from mechanical support despite antiarrhythmic drug therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Managing this critically ill group of patients is extremely challenging,” says Cleveland Clinic cardiologist Ayman Hussein, MD, senior author of the paper. “Ablation as a last resort proved to be a viable option, allowing liberation from mechanical hemodynamic support shortly afterward. At Cleveland Clinic, we are fortunate to have an excellent infrastructure that allows us to take care of these critically ill patients. Such results could only be achieved with the support and expertise of our colleagues in cardiac intensive care, cardiac surgery and heart failure medicine.”
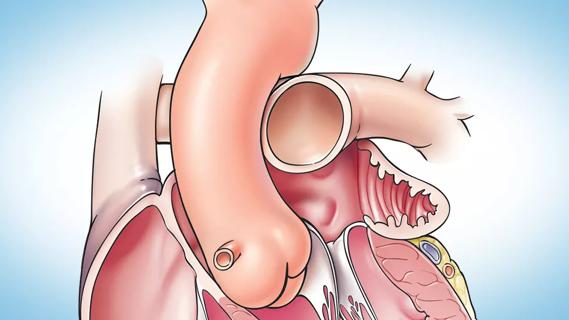
Patients on mechanical support with cardiogenic shock and ventricular arrhythmias that cannot be controlled with antiarrhythmic drugs have few options: either heart transplantation or bailout ablation of ventricular arrhythmia. VT ablation is especially difficult in this setting of hemodynamic compromise, which hampers the ability to maintain the arrhythmia long enough to allow for adequate mapping and ablation without further deterioration. Little evidence is available on outcomes of bailout ablation under these circumstances.
Consecutive patients with cardiogenic shock and concomitant refractory ventricular arrhythmia who underwent bailout ablation due to inability to wean off mechanical support were identified from a prospectively maintained Cleveland Clinic registry from 2010 to 2017.
Among the 21 patients identified, median age was 61 years, and 86% were male. Median left ventricular ejection fraction was 20%, and 81% had ischemic cardiomyopathy. Median PAINESD score, which predicts periprocedural acute hemodynamic decompensation in patients undergoing VT ablation, was 18 ± 5 (out of 35 maximum).
Advertisement
Mechanical support devices in place prior to the procedure were as follows:
Patients were maintained on a median of two antiarrhythmic drugs, with most (n = 14; 67%) on a combination of amiodarone and lidocaine. Others were on either amiodarone alone (n = 2), lidocaine alone (n =3), procainamide alone (n = 1) or amiodarone alone (n =1).
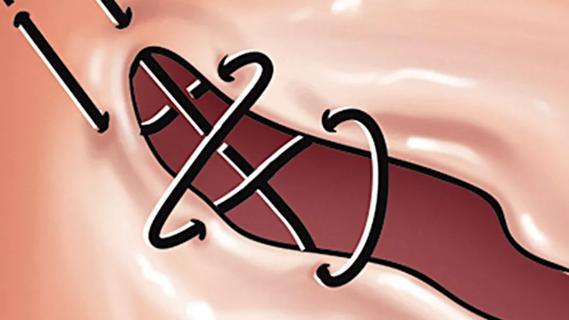
Clinical VTs were inducible and activation mapping was possible in 13 patients (62%). Six patients (29%) had premature ventricular contraction (PVC)-induced ventricular fibrillation/VT, and in two patients (9%), VT could not be induced.
The ablation procedures targeted the clinical VTs and PVCs in addition to empiric scar modification. At the end of the procedure, 91% of patients had no inducible VTs.
Overall, the following outcomes were found after VT ablation:
Outcomes among the 15 survivors included the following:
Advertisement
Dr. Hussein notes that mortality was related mostly to worsening cardiogenic shock. Comparing the 15 patients who survived to discharge with the other six patients revealed that survivors were more likely to be male (93% vs. 67%) and to have the following:
Patients presenting with VT before shock onset fared better than patients who subsequently developed VT after presenting in shock requiring hemodynamic support. Survivors and nonsurvivors did not differ in terms of likelihood of having ischemic versus nonischemic cardiomyopathy.
While the analysis is limited by its small size and retrospective design, the authors note that it is the only study they’re aware of that investigated VT bailout ablation in this high-risk setting.
“Our findings confirm that ablation bailout for ventricular arrhythmia can save lives in this situation,” observes co-author Oussama Wazni, MD, Section Head of Cardiac Electrophysiology at Cleveland Clinic. He adds, however, that because the study reflects practice in a tertiary care center with staff highly experienced in intensive care, VT ablation and cardiac surgery, the results may not be applicable to smaller or nontertiary care institutions.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
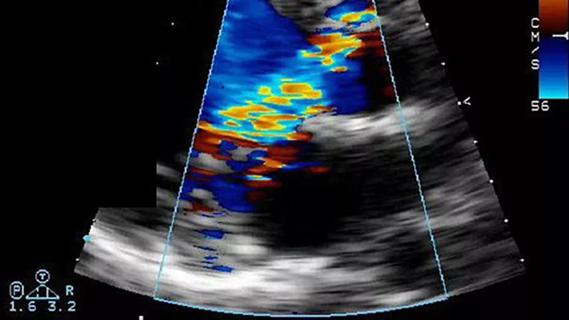
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
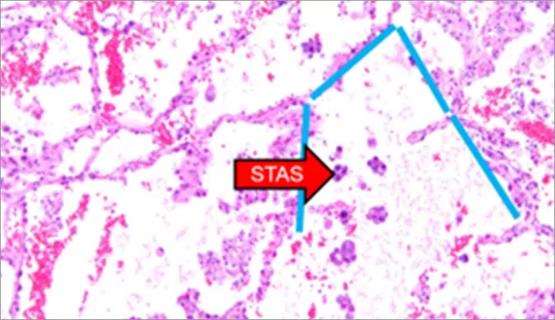
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable