Review of nearly 10,000 patients yields data on ideal effective dose for lowest risk of complications

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patients undergoing total joint arthroplasty (TJA) are at risk of developing venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE). Historically, without prophylaxis the rate of DVT in patients undergoing TJA was between 35 percent and 85 percent. Over time, surgical approaches and operative times improved dramatically; epidural and spinal anesthesia were chosen preferentially; pneumatic compression pumps were also introduced; and most importantly, patients were encouraged to mobilize earlier. Almost all physical therapy protocols today recommend same-day out-of-bed activities after surgery. With the introduction of these perioperative modifications, the incidence of VTE events underwent a dramatic reduction in clinically symptomatic DVTs and fatal PEs.
Recently, the incidence of VTE is reported to be less than 1 percent to 2 percent. With such a low incidence and the standardization of multimodal prophylaxis practices, it became difficult to distinguish differences in efficacy of different chemoprophylactic modalities.
There is a wide and expanding array of VTE chemoprophylactic agents for patients undergoing TJA. Potent agents, such as low-molecular-weight heparin (LMWH), warfarin or the newer anticoagulation agents have been the accepted practice. Many well-known challenges associated with these agents, such as the risk of bleeding and wound-related infections and difficulties with administration, titration and monitoring, were brought into scrutiny in the search for an ideal chemoprophylaxis.
Advertisement
Aspirin has long been established as an effective drug for preventing arterial thromboembolic events in cardiovascular and cerebrovascular diseases (low-dose 81mg). The role of aspirin as an effective modality for the prevention of VTE following TJA has been described in the medical literature for many decades. Aspirin is well tolerated, inexpensive and easy to administer with no need for routine blood monitoring.
With the endorsement of aspirin in many published guidelines (American Academy of Orthopaedic Surgeons 2009, 2011 and American College of Clinical Pharmacy 2012) and the additional emerging evidence demonstrating its efficacy, aspirin gained popularity in the orthopaedic community as an effective VTE prophylactic agent following TJA.
The only remaining question was about the optimal dose, and we endeavored to answer this question. If a regimen of 325 mg twice a day was efficacious (the current recommended regimen), would a smaller dose (81 mg twice a day) be equivalently efficacious given its pharmacodynamics and also have less risk of complications?
We retrospectively reviewed 16,000 medical records for primary TJA patients between 2012 and 2016. We identified 9,602 patients who received enteric-coated aspirin twice daily after surgery for four to six weeks depending on surgeons’ preference. A total of 2,360 patients received 81 mg (low-dose group) and 7,242 patients received 325 mg aspirin (high-dose group). Complications collected within 90 days after surgery were VTEs (DVT and PE), bleeding (gastrointestinal and wound bleeding) and mortality.
Advertisement
For patients who underwent total hip arthroplasty (THA), no statistical significant difference was observed between the aspirin groups in terms of VTE, DVT, PE, bleeding risk or mortality (Figures 1, 2). After adjusting for confounders, low-dose versus high-dose aspirin was not associated with increased risk for VTE, DVT, PE, bleeding or mortality after THA.
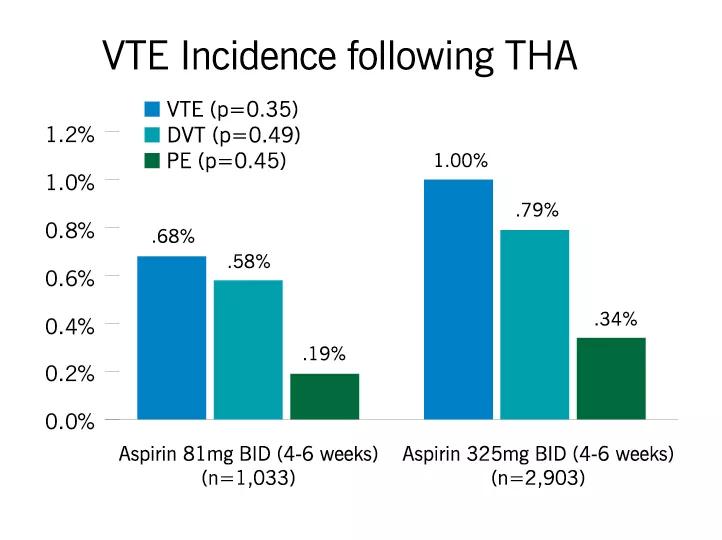
Figure 1: Incidence of venous thromboembolism (VTE), deep venous thrombosis (DVT) and pulmonary embolism (PE) within 90 days after total hip arthroplasty (THA).
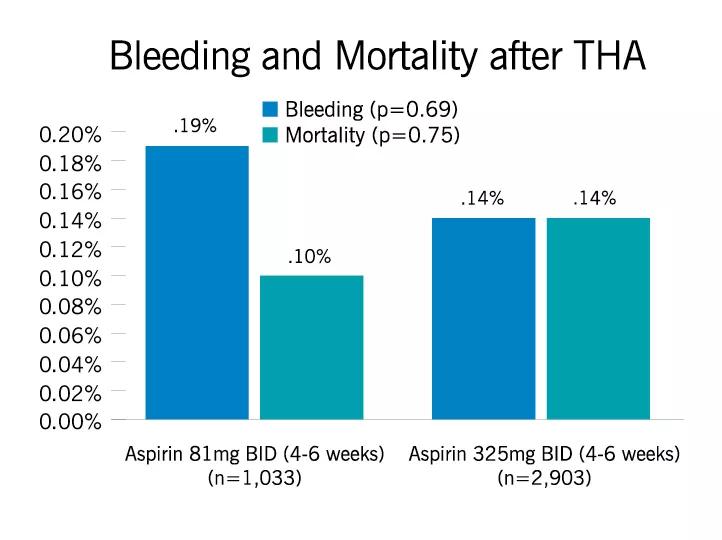
Figure 2: Incidence of bleeding (gastrointestinal and wound) and mortality within 90 days after total hip arthroplasty (THA).
For patients who underwent total knee arthroplasty (TKA), there were no statistically significant differences between the groups in term of VTE, PE, bleeding or mortality after surgery (Figure 3, 4). However, the incidence of DVT was lower in the low-dose aspirin group compared to high-dose group (0.53 percent versus 1.41 percent, respectively. p=0.01). Interestingly, low-dose aspirin was associated with reduced risk of DVT compared to high-dose aspirin in the regression model after accounting for confounders (OR=0.38, 95 percent CI [0.17 – 0.84], p=0.006). In addition, low-dose versus high-dose aspirin was not associated with increased risk of VTEs (p=0.10), PE (p=0.17), bleeding (p=0.79) or mortality (p=0.78) within 90 days after TKA.
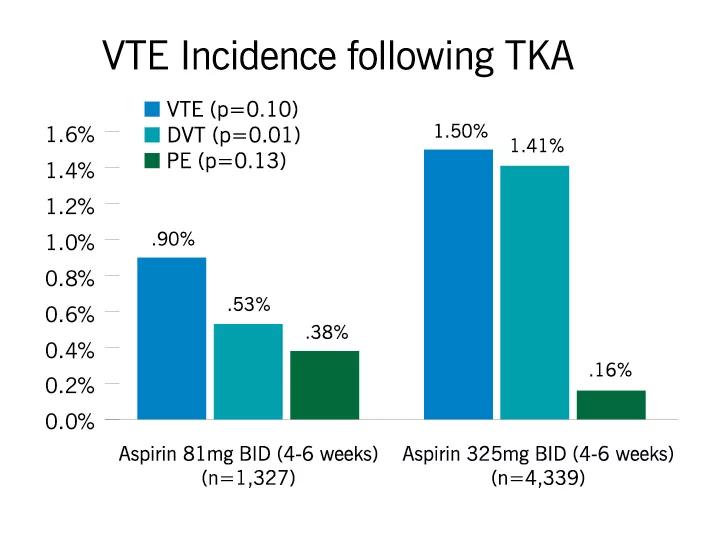
Figure 3: Incidence of venous thromboembolism (VTE), deep venous thrombosis (DVT) and pulmonary embolism (PE) within 90 days after total knee arthroplasty (TKA).
Advertisement
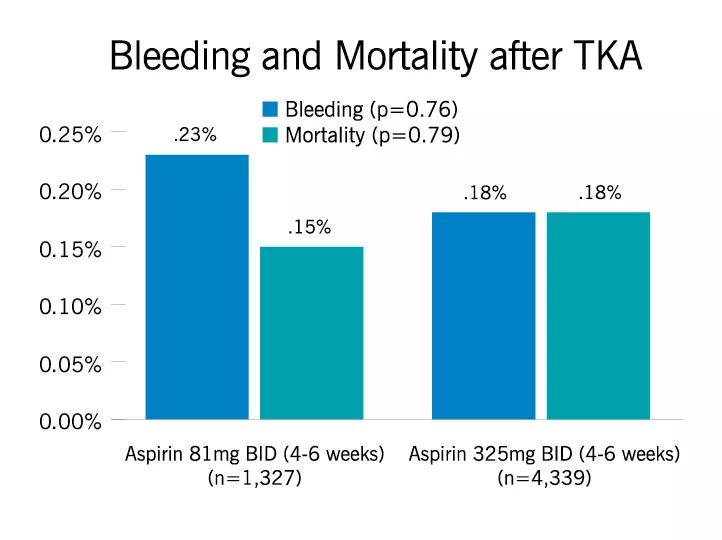
Figure 4: Incidence of bleeding (gastrointestinal and wound) and mortality within 90 days after total knee arthroplasty (TKA).
Overall, there was no difference in VTE incidence following TKAs/THAs in low-dose versus high-dose aspirin groups. Both aspirin regimens showed similar results in terms of risk of bleeding (GI and wound) and mortality after TJA.
We concluded that low dose of aspirin (81 mg twice a day) is not inferior to a higher dose of aspirin (325 mg twice a day) in the prevention of VTE following total hip and knee arthroplasty. We currently use ASA 81 mg PO BID for four weeks in primary arthroplasty procedures in low-risk patients.
Advertisement
Advertisement

Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients

How to diagnose and treat crystalline arthropathy after knee replacement

Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network

Reduced narcotic use is the latest on the list of robotic surgery advantages

Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals

Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions