Proposed model emerges from Cleveland Clinic data analysis

A team of Cleveland Clinic vascular surgeons has found that their practice is bucking the national trend toward decreased use of open aortic repair (OAR) for abdominal aortic aneurysms (AAAs), prompting a call for a national discussion around future directions for vascular surgery training.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The preservation of open aortic repair volumes in our program, and presumably at several other quaternary referral centers in the U.S., appears to offer a solution to the challenge of offering comprehensive vascular surgery training for aortic aneurysm treatment that includes open aortic repair as well as endovascular aneurysm repair [EVAR] and fenestrated endovascular aneurysm repair [FEVAR],” says Lee Kirksey, MD, MBA, Vice Chair of Cleveland Clinic’s Department of Vascular Surgery.
He is corresponding author of a study published in the Journal of Vascular Surgery that details Cleveland Clinic’s recent experience in AAA repair and suggests exploration of new training strategies to ensure adequate expertise in all repair strategies.
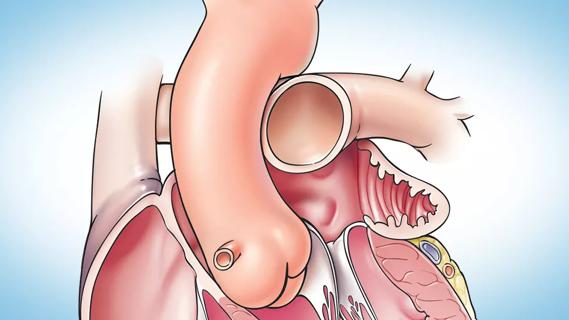
“Since the advent of the first generation of EVAR devices in the 1990s, there has been a paradigm shift in how infrarenal aneurysms are repaired,” notes Sean Lyden, MD, Chair of the Department of Vascular Surgery. He points to a recent review of Medicare data (J Vasc Surg. 2018;67:1690-1697) showing that open AAA repairs fell by 76% from 2003 to 2013 while EVAR volume nearly doubled.
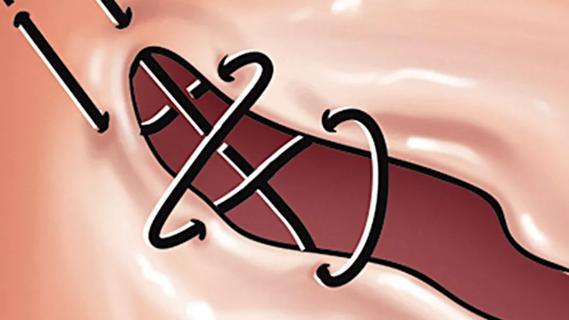
“Off-label treatment has allowed the expanded use of EVAR but has had clear implications for potential late failure,” says Dr. Lyden. “The release of custom commercial fenestrated devices and the completion of industry-sponsored trials for branched endovascular devices have allowed for on-label treatment of juxtarenal and thoracoabdominal aneurysms. The overall result is that many practicing surgeons are no longer doing enough open aortic surgery to maintain skills to do this well, and this leaves inadequate exposure and training for vascular surgery residents.”
Advertisement
“This trend away from open aortic surgery appeared to be at odds with our experience at Cleveland Clinic,” adds Dr. Kirksey, “so we set out to objectively confirm any such variance, reasons for the variance and potential implications for training at a national scale.”
To do so, he led a review of Cleveland Clinic’s entire procedural experience for patients with a diagnosis of AAA from 2010 through 2014. “We limited the analysis to Cleveland Clinic’s main campus quaternary hospital because all fenestrated and branched aortic repairs are performed there, and we were interested in examining the impact that other advanced repair options have on open repair volumes,” Dr. Kirksey explains.
Over the five years analyzed, 1,389 repair procedures were performed, breaking down as follows:
Notably, the total number of EVAR and FEVAR procedures done annually did not significantly change over time, whereas the annual number of OAR cases increased over the five-year period. In fact, there was a significant rise in the proportion of annual cases treated with OAR over time (P = 0.014).
Among the OAR cases, 59.3% involved juxtarenal aneurysms and 22.9% involved type IV thoracoabdominal aneurysms.
During the study period, Cleveland Clinic vascular surgery residents and fellows performed, on average, 23.1 OARs prior to their graduation. This compares with projections of less than 10 OARs, on average, for current graduating trainees nationwide.
Advertisement
“These findings confirm that we have seen a proportional increase in open repairs in recent years while our volumes for EVAR and FEVAR have remained stable,” says Dr. Kirksey. “We remain very comfortable with open techniques and limit off-label uses of endovascular methods.”
He adds that while these findings are counter to recent well-documented national trends, they are also congruent with those trends in some important ways. “We found that our open repairs are disproportionately composed of complex, technically challenging cases that demand advanced open aortic surgical skills, such as the more than 75% of our open cases that fall within the juxtarenal or suprarenal classifications,” he explains. “This suggests that as open repair volumes decline at most facilities across the nation, experience with the most challenging open repairs is diminishing, prompting more referral of complex AAA cases to experience-rich quaternary centers like ours.”
In their study report, Dr. Kirksey and co-authors write that they suspect this development will continue, likely resulting in what they call “regional complex aortic programs” to serve the needs of the vascular surgical community like similar programs have in disciplines including trauma and oncology.
“High-volume programs like this represent an opportunity to provide specialized training in both routine and complex open repairs as well as exposure to innovative endovascular techniques, such as in post-fellowship advanced aortic training,” says Dr. Kirksey. “Creating regionalized centers of excellence for open aortic surgery could centralize the provision of open aortic repair, with these centers serving as a hub for additional subspecialized training of residents and fellows — either optional or mandatory — in open repair and FEVAR. Certification in open repair could be offered for those who want it.”
Advertisement
He and his co-authors note that while detailed discussions about such a model are still needed at the regional and national levels, the need for vascular surgery training to evolve in this area is undeniable.
“Despite the overall decline in open repairs, it remains essential that vascular surgery trainees be facile with both open and endovascular aortic repair techniques,” Dr. Lyden concludes.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
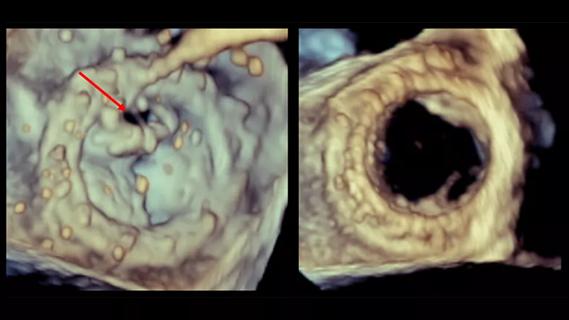
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
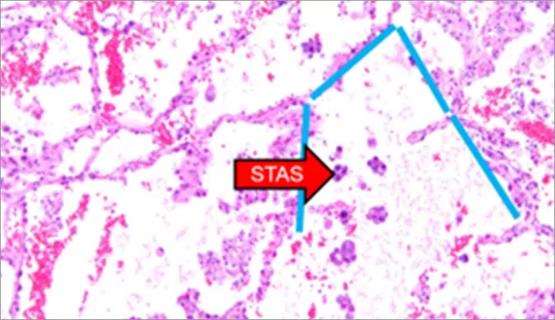
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
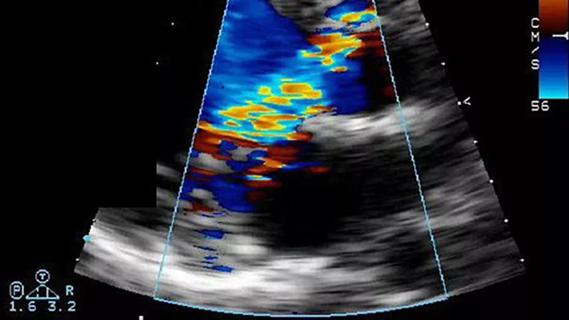
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable