When resourcefulness is needed at every turn
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 2015, a 56-year-old woman was transferred to Cleveland Clinic for management of acute onset of left arm ischemia. Three-dimensional (3-D) CT-reconstructed imaging showed a left subclavian aneurysm with embolization, a rare and potentially dangerous complication of arterial thoracic outlet syndrome (Figure 1).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/da44ec7c-ab13-485f-9e63-33fd1ed7953c/Lyden-Fig-1_jpg)
Figure 1. 3-D CT reconstruction at presentation showing the left subclavian aneurysm with embolization.
Because of the embolic burden in the outflow of the arm and hand, the initial strategy was catheter-directed pharmacologic thrombolysis. We used a dual-level infusion for thrombolysis with tissue plasminogen activator (t-PA). Progress of the therapy was checked eight hours after initiation. Minimal progress of the lysis was noted, and there was significant residual clot burden in the arm, so mechanical thrombectomy was performed with the Possis AngioJet™ device.
After mechanical thrombectomy, several areas of stenosis were uncovered in brachial and radial arteries. These were treated with percutaneous transluminal angioplasty, which improved flow to the arm. The patient was kept on therapeutic anticoagulation with planned resection of the subclavian artery aneurysm.
Despite anticoagulation, rethrombosis of the brachial and axillary arteries occurred six hours later. The patient was returned to the operating room, where she underwent open thrombectomy of the arteries from a brachial cutdown and local instillation of t-PA into the radial and ulnar arteries to improve outflow. The forearm was noted to be tense. Clinically, compartment syndrome was present and was the likely etiology of the rethrombosis. This was treated with forearm fasciotomy and carpal tunnel release. The hand perfusion was markedly improved by the repeat operation.
Advertisement
Elevation of the subclavian artery over a cervical rib leads to local arterial trauma, aneurysmal formation with thrombus deposition, and embolization to the distal extremity. For this reason, surgical correction of the arterial thoracic outlet pathology was performed a few days later. This included resection of the left cervical and first rib, resection of the aneurysm and reconstruction with a left subclavian-to-axillary artery graft using the right femoral vein. The operation was notable for a very friable and small proximal subclavian artery just distal to the left vertebral.
Duplex ultrasonography before discharge and at six-month follow-up intervals during the first year showed a widely patent bypass and equal upper extremity brachial pressures.
Although the patient had no symptoms, surveillance duplex ultrasonography after one year showed increased left subclavian artery velocities from 60 to 187 cm/s at the proximal anastomosis suggestive of a greater than 50 percent stenosis. Pulse volume recordings were consistent with new mildly dampened waveforms in the left arm, and a 10-mm Hg pressure drop was noted in the left brachial artery relative to the right. Findings were confirmed by CT angiography, and 3-D CT reconstruction clearly demonstrated a stenosis at the proximal anastomosis (Figure 2).
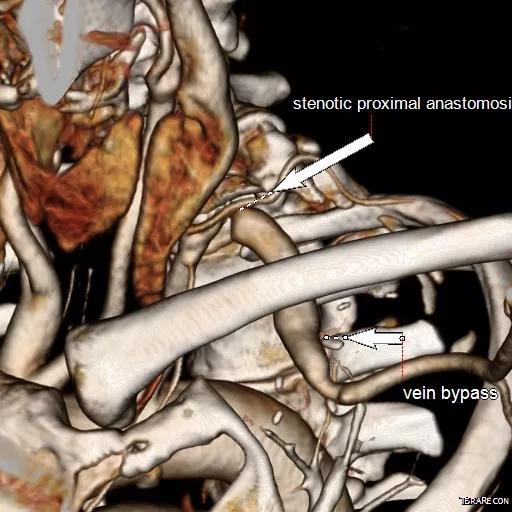
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c7f0961a-d14b-4a84-becd-2ddc0e12b341/Lyden-Fig-2_jpg)
Figure 2. 3-D CT reconstruction demonstrating stenosis at the proximal anastomosis one year after initial presentation.
Multiple options were available to treat this problem. Surgical revision was an option, but the reoperative nature and the small friable subclavian artery at the original operation made this the least appealing approach. Endovascular revision, the minimally invasive approach, was appealing to the physicians and patient. Several interventional options were considered:
Advertisement
A 6-mm-diameter, 17-mm-long stainless steel stent was used and was flared to 10 mm distally. The completion angiogram was normal (Figure 3).
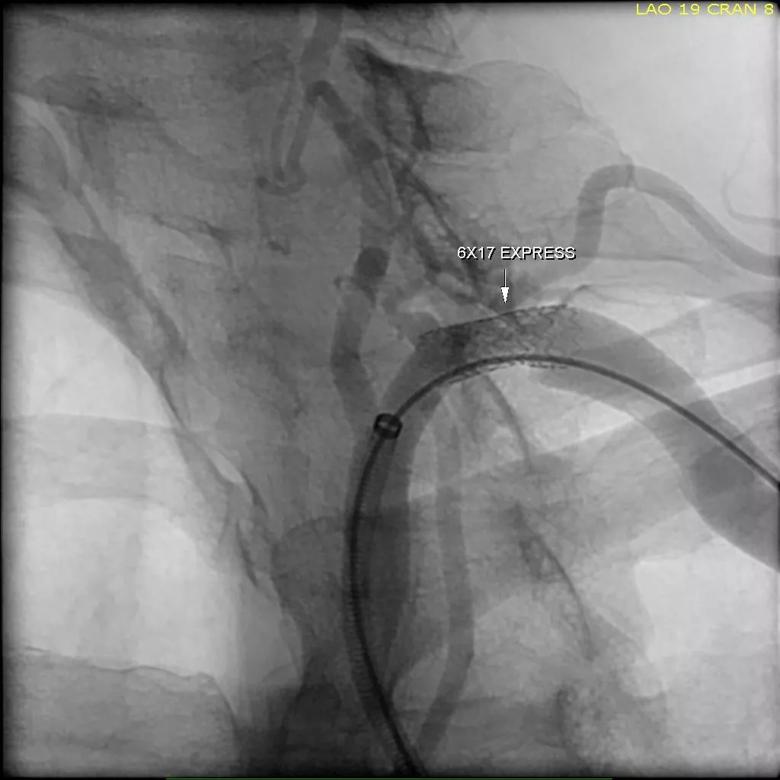
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d69824e-e147-47e0-911f-c15a631eaef3/Lyden-Fig-4_jpg)
Figure 3. Angiogram taken after stenting and flaring of the distal stent. Note the absence of residual stenosis.
The patient was discharged the same day on dual antiplatelet therapy and returned for office follow-up six weeks later with normalization of the duplex velocities, normal plethysmography and equal brachial pressures. We expect to continue to follow her for this problem for many years to come.
Dr. Lyden is Chair of Cleveland Clinic’s Department of Vascular Surgery.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable