New stent retrievers and patient-selection protocols promise less disability and death
A longtime hypothesis has now been confirmed with Level I, Class A evidence: Endovascular therapy can be highly beneficial in patients with acute ischemic stroke compared with IV t-PA alone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That’s the resounding message out of this year’s International Stroke Conference, where results of five randomized clinical trials — MR CLEAN, EXTEND-IA, ESCAPE, SWIFT PRIME and REVASCAT — were presented. The studies consistently showed that, compared with IV t-PA alone, endovascular therapy within six to eight hours after stroke onset:
The five studies are now published in the New England Journal of Medicine and represent the “turning of a historic corner” in acute stroke therapy, according to a statement from the National Institute of Neurological Disorders and Stroke.
The studies compared interventional therapy using new-generation mechanical thrombectomy devices (“stent retrievers” such as Medtronic’s Solitaire™ FR and Stryker’s Trevo®) vs. best medical management for acute ischemic stroke caused by large vessel occlusion, which represents a large subset of ischemic stroke cases.
The new studies put to rest lingering uncertainties about the efficacy of endovascular stroke therapy that arose from results of three trials released in 2013 that showed no advantage over IV t-PA alone. One of the key reasons for the shift in results since then appears to be related to the introduction of stent-retriever technology.
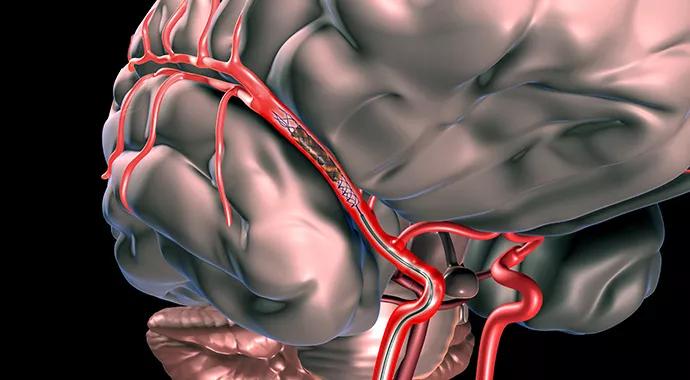
The new-generation catheter-based devices used in the latest studies deploy a metal mesh within the clot, in contrast to earlier devices that acquired control of the clot proximally or distally. The moment the mesh is deployed, a channel is opened to permit blood flow to starved brain tissue. The mesh expands to become one with the clot, allowing clot and mesh to be retrieved as a unit. The result is faster, more complete recanalization.
Advertisement
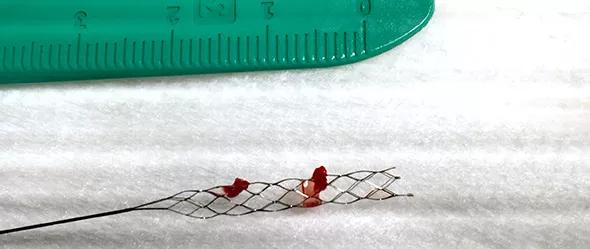
New-generation stent retrievers deploy a metal mesh within the clot, allowing clot and mesh to be extracted as a unit.
Another reason for the improvements in endovascular therapy outcomes is the use of better neuroimaging criteria for selection of endovascular therapy candidates.
Criteria in the latest studies are similar to those in the “hyperacute MRI protocol” used for the past several years by Cleveland Clinic’s Cerebrovascular Center. “This protocol promotes the use of advanced MRI techniques (in conjunction with CT or CT angiography) to enable more precise determination of tissue viability and occlusion impact before acute stroke intervention,” says Cerebrovascular Center specialist Gabor Toth, MD. This has allowed Cleveland Clinic stroke specialists to better select patients within traditional time windows for intra-arterial stroke therapy and to extend the window for acute interventional treatment.
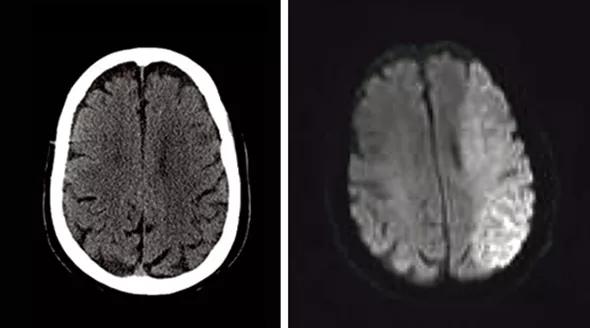
Left: Noncontrast brain CT without evidence of an acute infarct despite left middle cerebral artery (MCA) syndrome on examination. Right: Axial diffusion trace MRI in the same patient within 20 minutes, showing infarction of the entire left MCA territory.
The Cerebrovascular Center’s positive outcomes with this protocol have included the following, as reported recently in Stroke:
Advertisement
With the latest clinical trial data, a new era in endovascular stroke therapy is at hand — one where many more acute stroke patients can be saved from death or severe, lifelong disability.
Yet this new era has major implications for the delivery of acute stroke care. “Effective use of modern endovascular therapy devices demands that systems of care be in place to rapidly identify appropriate patients and swiftly get them to the neuroangiography suite for intervention,” says Dr. Toth.
To that end, Cleveland Clinic’s Cerebrovascular Center uses new-generation endovascular therapy devices on a daily basis in neuroangiography suites on Cleveland Clinic’s main campus as well as in regional hospitals on Cleveland’s east and west sides.
Their expert use of these technologies is enhanced by the following:
“We are committed to collaborating with colleagues in the community to offer these advantages to reduce the burden of stroke disability in our shared patient population,” says Dr. Toth.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade