Greatest benefits seen with combined thrombolytic and thrombectomy therapies
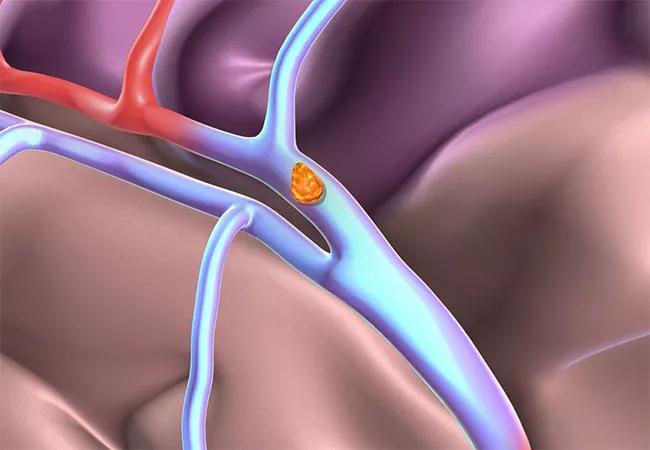
Among U.S. Medicare patients hospitalized with acute ischemic stroke from 2009 to 2013, 30-day mortality declined for those who received reperfusion therapies but not for those who did not, reveals a Medicare database analysis published by Cleveland Clinic researchers in the Journal of Stroke and Cerebrovascular Diseases (2019 Dec 10 [Epub ahead of print]). One-year mortality rates improved across the board during the same period, with particular improvement among patients who received reperfusion with intravenous thrombolysis (IVT), endovascular thrombectomy (EVT) or both.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Declining death rates from ischemic stroke coincided with the increasing use of acute reperfusion therapy,” says lead author Shumei Man, MD, PhD, a neurologist with Cleveland Clinic’s Cerebrovascular Center. “IVT and EVT were each associated with survival benefit, but the greatest advantage was evident for patients who received both therapies, followed by those receiving EVT.”
Over the past 20 years, stroke incidence and mortality rates have declined in the U.S. While reduced incidence has been attributed to a focus on managing cardiovascular risk factors, reasons for reduced mortality have not been well explored. Several randomized trials have shown that IVT and EVT, when given for acute ischemic stroke, improve functional outcomes, but epidemiologic assessment of the increasing use of these therapies has been lacking.
Data for the current analysis were drawn from the Medicare Provider Analysis and Review national database between January 1, 2009, and December 31, 2013. The study included 1,070,574 fee-for-service Medicare beneficiaries who were hospitalized with a primary diagnosis of acute ischemic stroke.
During the study period, the proportion of stroke patients treated with IVT ranged from 5.2% in 2009 to 8.3% in 2013, increasing by 60%. Treatment with EVT increased by 130% over the same period, but annual use rates were less than 1% during the entire period, reaching just 0.8% in 2013.
The study assessed trends in 30-day and one-year mortality following a stroke according to the acute therapies received, with multivariate logistic regression models generated to adjust for demographics and comorbidities.
Advertisement
Trends in 30-day mortality across the study period were as follows:
Trends in one-year mortality across the study period were as follows:
According to Dr. Man, benefits of the increased use of reperfusion therapy over time were clearly evident in the study. Moreover, each therapy was associated with incrementally increasing benefit over each year of the study. Technical advancements have been ongoing in EVT, which likely explains the improving trends for that therapy. And although there were no procedural changes in IVT during the study period, it is possible that quality improvement efforts shortened the time to IVT administration over time and perhaps broadened IVT use to include milder strokes.
The authors note that improvements in one-year mortality were seen among all groups, including those who received no reperfusion therapy at all. “This likely reflects changes over time in patient care following acute hospitalization,” says senior author Ken Uchino, MD, Director of Research and Education for Cleveland Clinic’s Cerebrovascular Center. “But it’s not known to what extent this is due to prevention of complications after stroke, prevention of stroke recurrence or other changes in healthcare that helped reduce death rates.” Regardless, one-year mortality improved the most among patients who received some form of acute reperfusion.
Advertisement
Notably, the study period preceded the publication of several pivotal trials that demonstrated improved outcomes from more modern methods of endovascular thrombectomy. “Use of these methods has increased since 2013,” Dr. Uchino observes, “and we would expect mortality rates to have further improved since then.”
Moreover, while the study adjusted for potential confounding factors such as age, sex, race and multiple comorbidities, the researchers could not adjust for stroke severity, and patients younger than 65 were not represented.
Despite these limitations, the study is very clear about a couple of key points: 93% of Medicare beneficiaries with acute ischemic stroke received no reperfusion therapy, and this was the only patient group that saw no gains in short-term mortality over the study period.
“Reperfusion therapy is still greatly underused,” says Dr. Man. “Our study indicates that quality improvement efforts to increase its use present a real opportunity to save more lives. More work can be done to make people aware of stroke signs and the need to call 911 early, as well as to streamline pre-hospital and in-hospital processes to provide timely reperfusion therapy to as many patients as possible.”
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade